Therapeutic basics of cardiovascular system & Drugs | MPO training 20
Understanding the therapeutic basics of cardiovascular system & drugs is a
key part of preparing for your journey as a Medical Promotion Officer (MPO).
This content introduces how cardiovascular conditions are managed through
different drug classes and mechanisms.
If you're planning to build a pharma career, this topic will help you
communicate medical knowledge clearly with healthcare providers. It presents
real insights that are essential for MPO training and fieldwork.
Table of contents: Therapeutic basics of cardiovascular system & Drugs
Check out the table of contents of this article and you can click on the part
you want to read from-
-
Part 1 : Therapeutic basics of cardiovascular system & Drugs
- What is Blood Pressure?
- Blood Flow in the Heart
- Cardiac Output
- Peripheral Vascular Resistance
- Blood Pressure: Controlling Factors
- Regulation of Blood Pressure Mechanisms
- Coronary Artery
- Different Lipids
- Medical Background Major Heart Diseases: Hypertension
- Ideal Antihypertensive: Qualities
- Anti - Hypertensive Drugs (Generic Name only)
- Difference: ACE Inhibitor & AT1 Receptor Blocker
- Difference: Non Selective & Cardioselective Beta- Blocker
- Angina: Treatment
- Drugs: Congestive Heart Failure
- Part 2 : Classification Chart With Brand and Generic
- FAQs
- Conclusion
Part 1 : Therapeutic basics of cardiovascular system & Drugs
The therapeutic basics of cardiovascular system & drugs includes how
different medicines help control heart diseases like hypertension,
arrhythmia, and heart failure. Medical Promotion Officers (MPOs) should know
how these drugs work to explain them to doctors effectively.
This knowledge helps you understand the purpose and effects of each drug
group used in cardiovascular care. It forms a foundation for your medical
communication skills.
What is the cardiovascular system and why is it important?
The cardiovascular system includes the heart and blood vessels. It delivers
oxygen and nutrients to the body and removes waste products. Its proper
function is vital for life.
What are the common cardiovascular diseases (CVDs)?
The most common CVDs include hypertension, heart failure, angina, myocardial
infarction (heart attack), and arrhythmias.
We will learn this article by dividing it into two parts. For example:
- Part 1 : Therapeutic Basic of Cardiovascular System & Drugs.
- Part 2 : Classification Chart With Brand and Generic.
Let's start the detailed discussion now.
What is Blood Pressure?
It is the lateral pressure exerted on the wall of the blood vessel by the
flowing blood.
Blood pressure is the force of blood pushing against the walls of arteries
as it flows through them.
Blood Flow in the Heart
Blood Flow in the Heart:
Our body needs oxygen to stay alive. The heart is the organ that pumps
oxygen-rich blood to every part of the body. It also brings back
oxygen-poor blood to send it to the lungs for fresh oxygen. Let’s
understand this step by step.
1. Oxygen-poor blood returns from the body to the heart
After delivering oxygen to different parts of the body, blood becomes
oxygen-poor. This blood returns to the heart through two large veins:
- From the upper body: Superior Vena Cava
- From the lower body: Inferior Vena Cava
This blood enters the Right Atrium (upper right chamber of the heart).
2. Blood goes to the lungs for oxygen
From the Right Atrium, the blood flows into the Right Ventricle (lower
right chamber).
The Right Ventricle then pumps the blood to the lungs through the
Pulmonary Artery.
In the lungs, the blood picks up fresh oxygen and releases carbon
dioxide.
3. Oxygen-rich blood comes back to the heart
The oxygen-rich blood returns from the lungs to the heart through the
Pulmonary Veins.
It enters the Left Atrium (upper left chamber).
4. Oxygen-rich blood is pumped to the whole body
From the Left Atrium, blood flows into the Left Ventricle (lower left
chamber).
The Left Ventricle is the strongest part of the heart. It pumps the
blood into the Aorta, the largest artery, which carries the oxygen-rich
blood to the entire body.
Quick Summary of the Blood Flow Path:
Body → Right Atrium → Right Ventricle → Lungs → Left Atrium → Left
Ventricle → Body
Important Valves in the Heart:
The heart has four main valves that keep the blood moving in the
right direction:
- Tricuspid Valve: Between Right Atrium and Right Ventricle
- Pulmonary Valve: Between Right Ventricle and Pulmonary Artery
- Mitral Valve: Between Left Atrium and Left Ventricle
- Aortic Valve: Between Left Ventricle and Aorta
Final Words: The heart works like a smart pump that keeps blood moving, delivering
oxygen and removing waste. This continuous blood flow is what keeps us
alive every second.
Quick Summary:
Cardiac Output
It is the amount of blood discharged by the left ventricles into the
aorta per minute.
It depends on:
- Blood Volume
- Venous Return
- Force of Contraction of Myocardium or Inotropic property
- Frequency of heart beat
Peripheral Vascular Resistance
It is the resistance offered by the blood vessel to the circulating
blood.
It depends on:
- Elasticity of Arterial Wall
- State of lumen of Blood Vessel
- Velocity of Blood
- Viscosity of Blood
Blood Pressure: Controlling Factors
Blood Pressure = Cardiac Output X Peripheral Vascular
Resistance.
- BP = CO X PVR
- BP = Blood Pressure
- CO = Cardiac Output
- PVR = Peripheral Vascular Resistance
BP can be increased or decreased depending on CO and PVR change.
Regulation of Blood Pressure Mechanisms
There are three main mechanisms involved in the regulation of Blood
Pressure.
They are:
- Nervous Mechanism
- Renin Angiotensin Aldosterone System (RAAS)
- Calcium Influx Mechanism
1) Nervous Mechanism
Sympathetic and parasympathetic nervous both can influence BP.
Sympathetic nervous system secretes hormones Epinephrine and
Norepinephrine.
They have:
- Vasoconstricting Effect
- Myocardial Contractility
- Heart Rate
2) Renin Angiotensin Aldosterone System (RAAS)
The RAAS is a hormone system that helps regulate blood pressure and
fluid balance in the body.
Step-by-Step Explanation:
Step 1: Drop in Blood Pressure or Blood Volume
- When there is a decrease in blood pressure or low fluid volume, the kidneys detect this change.
- In response, the kidneys release a hormone called Renin.
Step 2: Renin Converts Angiotensinogen into Angiotensin I
- The liver continuously produces a protein called Angiotensinogen.
- Renin acts on angiotensinogen and converts it into Angiotensin I.
Step 3: Angiotensin I is Converted to Angiotensin II
- In the lungs, an enzyme called ACE (Angiotensin-Converting Enzyme) is released.
- ACE converts Angiotensin I into Angiotensin II, which is the active form.
Step 4: Actions of Angiotensin II
Angiotensin II has two main effects:
- It causes vasoconstriction – narrowing of blood vessels, which increases blood pressure.
- It stimulates the adrenal glands to release Aldosterone.
Step 5: Aldosterone Acts on the Kidneys
- Aldosterone signals the kidneys to reabsorb salt (NaCl) and water (H₂O).
- This increases blood volume and helps raise blood pressure.
Final Result: Together, these steps restore blood pressure
and maintain fluid balance in the body.
In Short: Low BP → Renin ↑ → Angiotensin II ↑ →
Vasoconstriction + Aldosterone ↑ → NaCl + H₂O reabsorption → BP ↑
- Renin is an enzyme secreted by kidneys. Renin converts Angiotensinogen to active Angiotensin - I.
- Angiotensinogen is a plasma protein. It is secreted from the liver.
- Angiotensin is a hormone.
- Aldosterone is a hormone secreted by the Adrenal Cortex responsible for reabsorption of Na+(salt) and water.
- Angiotensinogen —> Renin —-> Angiotensin - I
- Angiotensin - I —--> ACE —> Angiotensin - II
ACE: Angiotensin Converting Enzyme.
Angiotensin - II increases blood pressure in two different
ways:
- Angiotensin - II is a potent vasoconstrictor. It increases secretion of Noradrenaline, a hormone from the adrenal gland. Noradrenaline constricts blood vessels.
- Angiotensin II increases reabsorption of both salt (Na+) and water. It increases secretion of aldosterone, a hormone, from the adrenal gland. Aldosterone also decreases excretion of salt and water from the body.
Calcium Influx Mechanism
Calcium ions play an important role in the contraction of
muscles of the heart and of the blood vessel.
- Rise in Ca2+ lon.
A rise in Calcium ion increases contraction of the cardiac and
vascular smooth muscles leading to increase in BP.
Decrease in Ca2+ lon:
- A decrease in calcium ion lowers the contraction of Cardiac and
- vascular smooth muscle leading to decrease in BP.
Calcium ion (Ca2+) Influx in Cardiac Muscle:
Effect of Calcium Ion (Ca²⁺) in Cardiac Muscle-
- When calcium ions (Ca²⁺) enter the cardiac muscle.
- They make the heart muscle contract more strongly.
- This causes the heart rate to increase.
- As the heart pumps faster and harder, the cardiac output (amount of blood pumped per minute) goes up.
- As a result, the blood pressure increases.
In short: More calcium → stronger heart contractions
→ faster heartbeat → more blood pumped → higher blood
pressure.
Calcium ion Influx in Vascular Smooth Muscle:
Effect of Calcium Ion (Ca²⁺) in Vascular Smooth Muscle -
- When calcium ions (Ca²⁺) enter the smooth muscles of blood vessels.
- The blood vessels contract or become narrower – this is called vasoconstriction.
- As the vessels get narrower, it becomes harder for blood to flow, which increases resistance.
- This increased resistance leads to a rise in blood pressure (BP).
In short: Ca²⁺ enters → vessels constrict → resistance
increases → blood pressure goes up.
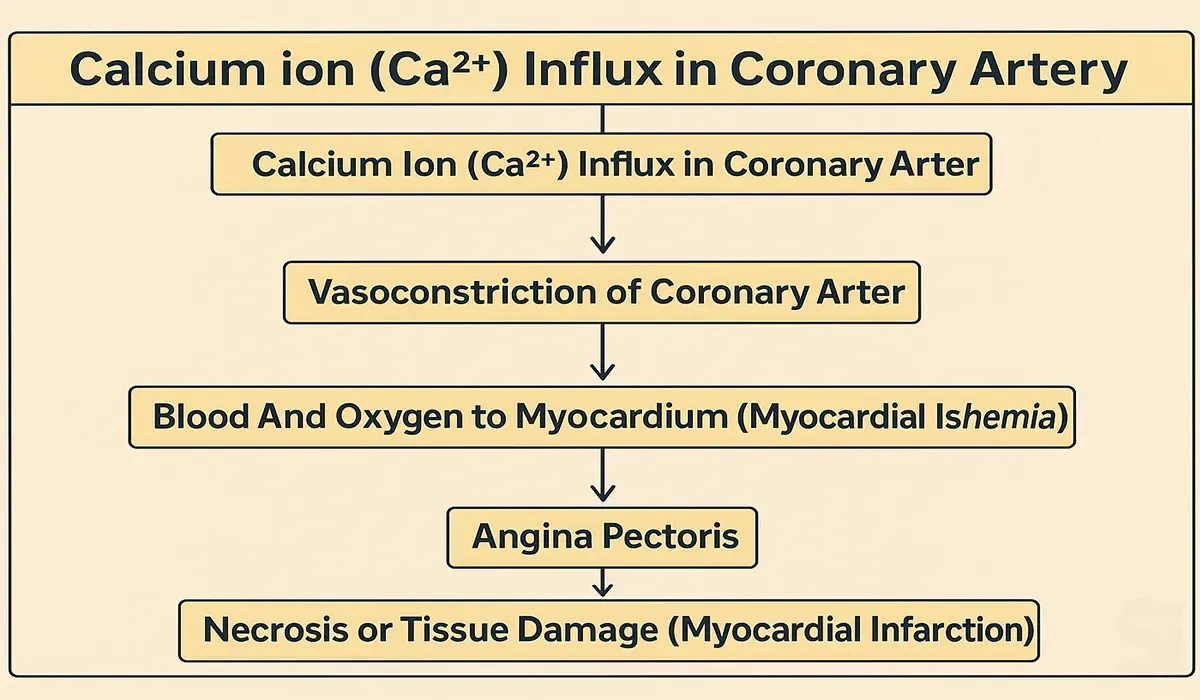
Calcium ion (Ca2+) Influx in Coronary Artery:
What the image explains in simple terms -
- When calcium ions (Ca²⁺) enter the coronary arteries in large amounts.
- The blood vessels become narrow (this is called vasoconstriction).
- As a result, less blood and oxygen reach the heart muscles.
- This causes chest pain, also known as angina.
- If this continues for a long time, it can lead to damage or death of heart tissue, which is called a heart attack (myocardial infarction).
In short: More calcium → narrowed blood vessels → less
blood to heart → chest pain → heart attack.
This is a step-by-step process of how excess calcium can harm the
heart.
Coronary Artery
Coronary Artery: Coronary artery is a major blood vessel
in our body -that supplies blood to the heart muscle.
The heart muscles need the oxygen and nutrients in blood so they
can pump blood through the heart and the rest of your body.
There are two coronary arteries, each containing several
branches:
Right coronary artery (RCA): The RCA supplies blood to
the right atrium and right ventricle. Its branches supply the
sinoatrial (SA) and atrioventricular (AV) nodes. These nodes
send electrical signals through the heart, so the heart muscles
know when to contract.
Left main coronary artery (LMCA): The LMCA supplies blood
to the left atrium and left ventricle. Its branches supply blood
to the other two-thirds of the interventricular septum.
Different Lipids
Lipid: The lipid is the building block of fatty
substances. They are mainly composed of cholesterol, protein and
triglyceride. protein and triglyceride. ই Lipids play important
role in many physiological functions including the maintenance
of normal metabolism and cellular structure.
Triglyceride: Triglycerides are a type of fat. They are
the most common type of fat in your body. They come from foods,
especially butter, oils, and other fats we eat. Triglycerides
also come from extra calories. Our body changes these extra
calories into triglycerides and stores them in fat cells. When
our body needs energy, it releases triglycerides.
Lipoprotein: A lipoprotein is a biochemical substance
whose purpose is to transport lipid molecules in the blood.
Cholesterol: A waxy, fat-like substance made in the liver
and found in the blood and in all cells of the body.
Cholesterol is an essential component of cell membranes, brain
and nerve cells and of bile, which helps the body absorb fats
and fat-soluble vitamins. The body uses cholesterol to make
vitamin D and various hormones, such as estrogen, testosterone
and cortisol.
The three main types of cholesterol include:
LDL-Low Density Lipoprotein: "Bad" cholesterol. Having
high levels of LDL cholesterol can lead to plaque buildup in our
arteries and result in heart disease or stroke.
HDL-High Density Lipoprotein: "Good" cholesterol. HDL is
known as "good" cholesterol because high levels can lower our
risk of heart disease and stroke.
VLDL-Very Low Density Lipoprotein: The VLDL particles
mainly carry triglycerides. VLDL is similar to LDL cholesterol,
but LDL mainly carries cholesterol to your tissues instead of
triglycerides.
Total Cholesterol: The total amount of cholesterol in our
blood based on our HDL, LDL and triglycerides numbers.
Desirable Cholesterol Levels:
| Total cholesterol | Less than 200 mg/dL |
| LDL ("bad") cholesterol | Less than 100 mg/dL |
| HDL ("good") cholesterol | Greater than or equal to 60 mg/dL |
| Triglycerides | Less than 150 mg/dL |
Medical Background Major Heart Diseases: Hypertension
What is called Hypertension?
Hypertension: Hypertension is known as high blood pressure. It is a
long-term medical condition in which the blood pressure in the blood
vessels remains continuously high.
Long-term high blood pressure, however, is a major risk factor for
coronary artery disease, stroke, heart failure, atrial fibrillation,
peripheral arterial disease, vision loss, chronic kidney disease, and
dementia.
Hypertension: Grades
| Category | Systolic (mm Hg) | and/or | Diastolic (mm Hg) |
|---|---|---|---|
| Normal | Less than 120 | and | Less than 80 |
| Elevated | 120-129 | and | Less than 80 |
| Category | Systolic (mm Hg) | and/or | Diastolic (mm Hg) |
|---|---|---|---|
| Stage 1 | 130-139 | or | 80-89 |
| Stage 2 | 140 or higher | or | 90 or higher |
| Hypertensive Crisis | Higher than 180 | and/or | Higher than 120 |
Primary Hypertension: Hypertension which has unknown cause is
called primary hypertension or Essential hypertension or Idiopathic
tension.
Secondary Hypertension: Hypertension which has known cause is
called is called Secondary hypertension.
Hypertensions: Complications
Untreated hypertension can lead to the following medical conditions:
A. Heart and blood vessel
- Arteriosclerosis/atherosclerosis
- Heart attack
- Stroke
- LVH (Left Ventricular Hypertrophy)
- Heart failure
- Hypertensive encephalopathy
B. Eye
- Hypertensive retinopathy
C. Kidney
- Kidney damage / Renal failure
Ideal Antihypertensive: Qualities
- Able to control all grades of hypertension.
- Should not develop tolerance.
- Effective even in monotherapy.
- Regression of LVH.
- Should not affect metabolic profile.
- Long term Safety data.
- Can be given in different concomitant diseases along with hypertension.
- P/T Ratio will be more than 50%.
- Should provide gradual onset of action rather than quick onset action.
- Should be long acting rather than short acting.
- Should not affect routine life.
Anti - Hypertensive Drugs (Generic Name only)
1. ACE Inhibitors : Lisinopril, Captopril, Enalapril
2. AT1 Receptor Blocker ARB : Losartan, Olmesartan, Irbesartan
3. Calcium Channel Blockers : Amlodipine, Nifedipine
4. Beta Blockers :
- a. Non Selective : Propranolol
- b. Cardio selective : Atenolol, Bisoprolol
4. Alpha-beta blockers : Carvedilol
5. Diuretics : Hydrochlorothiazide, Furosemide, Spironolactone
6. Vasodilators : Isosorbide mononitrate
7. Lipid Lowering Agent : Atorvastatin, Rosuvastatin, Simvastatin
8. Antiplatelet Agent : Clopidogrel, Aspirin
Difference: ACE Inhibitor & AT1 Receptor Blocker
| ACE Inhibitor | AT1 Receptor Blocker |
|---|---|
| Inhibit ACE | Blocks Angiotensin II |
| Increases the level of kinins and other autacoids like Bradykinin and prostaglandin | Doesn't do like this |
| Possibility of causing Dry cough | Doesn't do like this |
| Captopril, Lisinopril, Enalapril | Losartan, Olmesartan |
Difference: Non Selective & Cardioselective Beta- Blocker
| Sl. No. | Cardioselective | Non-Cardioselective |
|---|---|---|
| 01 | Acts on beta receptor present in heart and vascular smooth muscle | Acts on beta receptor present in Lung and heart and vascular muscle |
| 02 | Do not cause asthma | Can cause asthma |
| 03 | Not contraindicated in asthma | Contraindicated in asthma |
| 04 | Atenolol | Propranolol |
Carvedilol: More than a beta-blocker
- Dual acting alpha and beta blocking agent. So it reduces PVR and are suitable for CHF with Hypertension.
Angina: Treatment
1. Beta-blockers:
- a. Non Cardioselective - Propranolol
- b. Cardioselective - Atenolol, Bisoprolol
2. Vasodilators:
- a. Isosorbide mononitrate
3. Calcium Channel Blockers
- Amlodipine, Nifedipine
4. Anti-Platelet Aggregator
a. Salicylic acid
Drugs: Congestive Heart Failure
1. Cardiac Glycosides: Provides positive inotropic effect and
increases CO.
2. ACE Inhibitors: Increases cardiac out by reducing preload and
afterload.
3. Diuretics: Decreases preload by reducing blood volume.
4. Vasodilators: Decreases afterload and increases CO.
Part 2 : Classification Chart With Brand and Generic
| Sl. No | Sub Class | Therapeutic Group |
|---|---|---|
| 1 | Antihypertensive |
a) Angiotensin II Receptor Blockers (ARB) b) Calcium Channel Blocker (CCB) c) Beta Receptor Blocker d) Diuretic e) Angiotensin Converting Enzyme (ACE) Inhibitors |
| 2 | Antianginal | a) Nitrates b) Fatty Acid Oxidation Inhibitor |
| 3 | Lipid Lowering |
a) HMG CoA Reductase Inhibitors (Statins) b) Fibrates |
| 4 | (Not Specified) | a) NSAID b) Antiplatelet (Antithrombotic) |
CVS Combination Drugs:
1. Antihypertensive
- a) ARB + CCB
- b) ARB + Diuretic
- c) CCB + Beta Blocker
2. Blood Thinner
- a) NSAID + Antiplatelet (Antithrombotic)
1. Antihypertensive Drugs
| Therapeutic Group | Total | Generic With Brand Name (ACME) |
|---|---|---|
| a) ARB | 3 | Losartan Potassium (Losart), Olmesartan Medoxomil (Orbas), Telmisartan (Telisa) |
| b) CCB | 2 | Cilnidipine (Duocard), Amlodipine (Amlopin) |
| c) Beta Receptor Blocker | 2 | Atenolol (Tenoloc), Bisoprolol (Betabis) |
| d) Diuretic | 1 | Spironolactone + Furosemide (Edemide) |
| e) ARB + CCB | 2 | Telmisartan & Amlodipine (Telisa-A), Olmesartan & Amlodipine (Orbapin) |
| f) ARB + Diuretic | 2 | Losartan Potassium + Hydrochlorothiazide (Losart plus), Olmesartan medoxomil & Hydrochlorothiazide (Orbas Plus) |
| g) CCB + Beta Blocker | 2 | Amlodipine + Atenolol (Amloten), Amlodipine + Bisoprolol (Betabis A) |
| (h) Beta blocker + diuretic | 1 | Betabis plus (Bisoprolol) |
2. Antianginal Drugs
| Therapeutic Group | Total | Generic With Brand Name (ACME) |
|---|---|---|
| a) Nitrates | 1 | Nitroglycerin (Angist SR) |
| b) Fatty Acid Oxidation Inhibitor | 1 | Trimetazidine HCI (Angirid MR) |
3. Lipid Lowering Drugs
| Therapeutic Group | Total | Generic With ACME's Brand Name |
|---|---|---|
| a) HMG CoA reductase inhibitors/Statins | 2 | Atorvastatin (Liptor), Rosuvastatin (Rostab) |
| b) Fibrates | 1 | Fenofibrate (Lipidof) |
4. Antiplatelet/Antithrombotic/Blood Thinner
| Therapeutic Group | Total | Generic With ACME's Brand Name |
|---|---|---|
| a) NSAID | 1 | Aspirin (Ecosprin) |
| b) Antiplatelet (Antithrombotic) | 1 | Clopidogrel (Dclot) |
| c) NSAID + Antiplatelet (Antithrombotic) | 1 | Aspirin + Clopidogrel (Ecosprin Plus) |
FAQs for Therapeutic Basics of Cardiovascular System & Drugs
1. What does “therapeutic basic” mean in cardiology?
It refers to the basic treatment principles used to manage
cardiovascular conditions using medicines and lifestyle changes.
2. What types of drugs are used to treat heart diseases?
Major types include antihypertensives, beta-blockers, calcium channel
blockers, ACE inhibitors, diuretics, statins, and anticoagulants.
3. How do beta-blockers work in heart treatment?
Beta-blockers slow down the heart rate and reduce blood pressure,
helping the heart to work more efficiently.
4. What is the role of ACE inhibitors?
ACE inhibitors help relax blood vessels, lower blood pressure, and
reduce the workload on the heart. They are often used in heart failure
and high blood pressure.
5. What is the difference between diuretics and statins?
Diuretics help remove excess fluid from the body, lowering blood
pressure. Statins reduce cholesterol levels to prevent heart attacks
and strokes.
6. Are side effects important to know for cardiovascular drugs?
Yes, Doctors often ask about side effects, and you must be ready to
answer. Common side effects include dizziness, cough, fatigue, or
swelling.
Conclusion
Mastering the therapeutic basic of cardiovascular system & drugs
gives you a strong foundation for working as an effective Medical
Promotion Officer (MPO). From drug types to their specific uses, this
knowledge connects medical science with real-world applications. It
helps you support healthcare professionals with correct information.
For every MPO in training, this is an essential step toward becoming
confident and informed in the pharmaceutical field.