Basic information about antibiotics and generic drugs | MPO training 17
Curious about antibiotics and generic drugs before starting your MPO journey?
This post covers the basic information about antibiotics and generic drugs
with real-world context tailored for future Medical Promotion Officers.
It’s written in plain language, so you can read and understand it in one go.
From definitions to examples, this article helps you connect the dots easily.
Whether you're preparing for an interview or just learning, this resource is
made for you.
Table of contents: Basic information about antibiotics and generic drugs
Take a look at everything you can know about antibiotics and generic drugs-
- Basic information about antibiotics and generic drugs
- Therapy-Resistance-Carrier Stage
- Post-Antibiotic Effect
- Properties of an Ideal Antibiotic
- Minimum inhibitory and bacterial concentration
- Penicillin antibiotics explain in details
- Cephalosporins generations antibiotic explain in details
- Macrolides generations antibiotic explain in details
- Fluoroquinolone generations antibiotic explain in details
- Aminoglycosides antibiotics explain in details
- Tetracycline antibiotics explain in details
- Meropenem antibiotics
- Classification Chart With ACME Brand and Generic
- Indication Chart of Antibiotic Generic
- Oral & Parenteral Antibiotic Brands of ACME Laboratories Ltd.
- FAQs about basic information about antibiotics and generic drugs
- Conclusion
Basic information about antibiotics and generic drugs
Every Medical Promotion Officer (MPO) needs a clear idea of how antibiotics
work and why generic drugs matter. This article breaks down the basic
information about antibiotics and generic drugs into simple points with
examples.
You’ll learn how these medicines are used in real practice and why
understanding generics gives you an edge in pharma sales. Designed for
beginners, this guide helps you start strong in your MPO career.
What are antibiotics?
*Antibiotics are medicines that fight infections caused by bacteria. They
either kill the bacteria or stop them from growing.
*Antibiotics are substances produced by microorganisms, or similar products
produced by bacterial chemical synthesis and are able to inhibit or kill
microorganisms without affecting the host.
History of Antibiotic
In 1929, Sir Alexander Fleming, a Scottish bacteriologist, went on a
vacation and left a petri dish of staphylococci bacteria uncovered. When he
returned, he noticed that there was mold growing on it. Upon further
examination, he saw that the area around the mold had no bacteria growing.
He named the mold Penicillium, and the chemical produced by the mold was
named penicillin, which is the first substance recognized as an antibiotic.
What are some common types of antibiotics?
Some commonly used antibiotic classes include penicillins, cephalosporins,
macrolides, tetracyclines, and fluoroquinolones.
Now we will learn all the details about antibiotics and generic names below.
Classification of Antibiotic
- Chemical Classification (Group of Antibiotic)
- Classification on the basis of Mechanism of Action
- Classification on the basis of Way/Nature/Effects of Activity
- Classification on the basis of Spectrum of Activity
1. Chemical Classification (Group of Antibiotic)
a. Beta-lactam antibiotics
-
a. Penicillin
- Natural Penicillin i.e. Phenoxymethyl Penicillin
- Semi synthetic Penicillin i.e. Amoxicillin ((Moxilin)
- b. Cephalosporin
- c. Carbapenem : Imipenem, Meropenem (Fulspec)
b. Macrolides : Erythromycin (Erocin), Azithromycin (Azin)
c. Fluoroquinolones : Ciprofloxacin (Cipro-A), Levofloxacin
(Leo)
d. Tetracycline : Doxycycline (Doxy-A), Oxytetracycline.
e. Aminoglycosides : Amikacin, Gentamicin
f. Sulfonamides : Co- Trimoxazole (sulfamethoxazole and
trimethoprim)
g. Polypeptides : Polymyxin B Sulphate, Colistimethate Sodium
(Xylistin)
h. Amphenicol : Chloramphenicol (A-Phenicol)
2. Classification on the basis of Mechanism of Action (Antibiotics)
A. Cell wall Synthesis Inhibitor
- Beta Lactam
B. Protein Synthesis Inhibitor
- Tetracycline
- Aminoglycoside
- Macrolide
- Amphenicol
C. Nucleic Acid Synthesis Inhibitor
- Fluoroquinolone
- Sulfonamide
- D. Cell Membrane Disruptor
- Polypeptides
Examples:
A. Inhibit Cell Wall Synthesis
1. Beta Lactam Antibiotics:
-
a. Penicillin:
- i. Natural Penicillin : Phenoxymethyl Penicillin
- ii. Semisynthetic Penicillin : Flucloxacillin (A-Flox)
- b. Cephalosporin:
- 1st generation: Cephradine (Sefril), Cephalexin.
- 2nd generation: Cefaclor(Alclor), Cefuroxime (Famicef)
- 3rd generation: Ceftriaxone (Trizon), Cefixime (Fix-A)
- 4th generation: Cefepime (Superpime)
-
C. Carbapenem:
- Meropenem (Fulspec), Imipenem
B. Inhibit Protein Synthesis
1. Tetracycline:
- Oxytetracycline
- Doxycycline (Doxy-A)
2. Aminoglycoside:
- Amikacin
- Gentamicin
3. Macrolide:
- Erythromycin (Erocin)
- Azithromycin (Azin)
4. Amphenicol:
- Chloramphenicol (A-Phenicol)
C. Inhibit Nucleic Acid Synthesis
1. Fluoroquinolone:
- Ciprofloxacin (Cipro-A)
- Levofloxacin (Leo)
D. Cell Membrane Disruptor
1. Polypeptides:
- Polymyxin B Sulphate
- Colistimethate Sodium (Xylistin)
3. On The Basis of Way/Nature/Effects of Activity
Bactericidal: Antibiotics that kill the bacteria. Examples:
Penicillin, Cephalosporins, Carbapenem, Fluoroquinolones,
Colistimethate Sodium etc.
READ MORE: Concept microbiology guide | MPO training 15
Bacteriostatic: Antibiotics that inhibit the growth of the
bacteria. Examples: Tetracyclines, Sulfonamides, Trimethoprim,
Macrolides, etc.
Cephalosporin Generation
1) 1st Cephalosporin Generation
- Cephradine (Sefril)
- Cefadroxil (Twicef)
2) 2nd Cephalosporin Generation
- Cefaclor (Alclor)
- Cefuroxime (Famicef
3) 3rd Cephalosporin Generation
(Oral):
- Cefixime (Fix-A)
- Cefpodoxime (CP)
- Ceftibuten (Logibac)
Parenteral:
- Ceftriaxone (Trizon)
- Ceftazidime (Trizidim)
4) 4th Cephalosporin Generation
- Cefepime (Superpime)
Beta-lactam
Beta-lactam:
- It is a chemical ring.
- This ring is present in Penicillin, Cephalosporin & Carbapenem.
- This ring is responsible for the bactericidal (kill bacteria) action.
Beta-lactamase:
- An enzyme.
- Produced by bacteria.
- Helps bacteria to destroy Beta-lactam rings in Penicillin, Cephalosporin and Carbapenem.
Beta Lactam Antibiotics
Antibiotics having Beta lactam ring in their structure are
called Beta Lactam antibiotics.
Example:
- Penicillin: Amoxicillin, Flucloxacillin
- Cephalosporin: Cephradine, Ceftriaxone
- Carbapenem: Meropenem
1. Inhibition of Cell Wall Synthesis:
- Examples: Beta-lactams, Glycopeptides, Bacitracin, Isoniazid.
- How they work: These antibiotics prevent bacteria from forming their protective cell wall, making them vulnerable and eventually causing cell death.
2. Disruption of Cell Membrane:
- Example: Lipopeptides.
- How they work: These antibiotics damage the bacterial cell membrane, leading to leakage and cell death.
3. Inhibition of DNA Gyrase (DNA Replication):
- Examples: Quinolones, Novobiocin.
- How they work: They block enzymes involved in DNA replication, stopping bacterial reproduction.
4. Inhibition of RNA Synthesis:
- Examples: Ansamycins, Pleuromutilins, Oxazolidinones.
- How they work: These antibiotics block the transcription process, so the bacteria cannot make essential proteins.
5. Inhibition of DNA-dependent RNA Polymerase:
- Example: Rifamycins.
- How they work: They prevent the enzyme that converts DNA into RNA from functioning properly.
6. Inhibition of Protein Synthesis (30S and 50S Ribosomal
Subunits):
- Examples: Tetracyclines, Aminoglycosides, Macrolides, Clindamycin.
- How they work: They target bacterial ribosomes and stop protein production, which is crucial for survival.
7. Inhibition of Folate Synthesis Pathway:
- Antibiotics interfere with the conversion of PABA → DHF → THF, a pathway necessary for DNA and RNA synthesis.
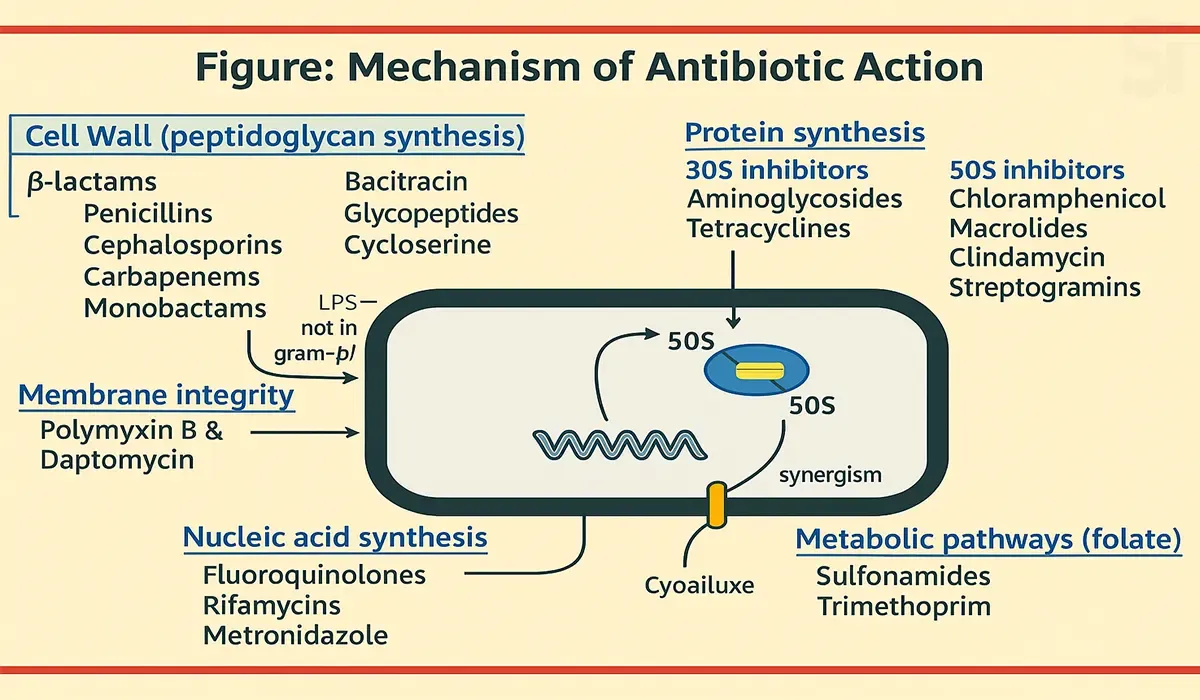
This diagram illustrates how different antibiotics target essential
components and processes within bacterial cells to stop their growth
or kill them.
Here's a clear and simple breakdown:
1. Inhibition of Cell Wall Synthesis
- Antibiotics: Glycopeptides, Beta-lactams.
- Mechanism: These antibiotics prevent bacteria from forming their protective cell wall, making them weak and leading to cell death.
2. Inhibition of DNA Replication
- Antibiotic: Quinolones.
- Mechanism: Quinolones block the bacterial enzymes responsible for DNA replication, stopping the bacteria from multiplying.
3. Interference with RNA Base Pairing
- Target: RNA base-pairing
- Mechanism: Disruption of RNA synthesis prevents proper genetic instructions from forming, which is essential for protein production.
4. Disruption of Protein Synthesis (Ribosome 30S Subunit)
- Antibiotic: Spectinomycin.
- Mechanism: This antibiotic binds to the 30S subunit of bacterial ribosomes and stops protein production, which is vital for bacterial survival.
5. Damage to Cytoplasmic Membrane Structure
- Target: Cytoplasmic Membrane.
- Mechanism: Antibiotics targeting the cell membrane cause leakage of cell contents, leading to cell death.
In Summary:
The image shows that antibiotics attack bacteria by:
- Breaking down the cell wall,
- Blocking DNA and RNA synthesis,
- Interfering with ribosome function,
- Damaging the cell membrane.
Each mechanism ultimately prevents the bacteria from growing or
causes it to die — making antibiotics powerful tools in fighting
infections.
This diagram explains how antibiotics work by targeting key structures
and functions in bacteria to stop their growth or kill them.
Here's a breakdown in simple terms:
1. Inhibition of Cell Wall (Peptidoglycan) Synthesis
- Antibiotics: β-lactams (Penicillins, Cephalosporins, Carbapenems, Monobactams) Bacitracin, Glycopeptides, Cycloserine.
- How it works: These antibiotics block the formation of the bacterial cell wall, weakening the bacteria and causing them to burst.
2. Disruption of Membrane Integrity
- Antibiotics: Polymyxin B, Daptomycin.
- How it works: These drugs damage the bacterial membrane, causing leakage of cell contents and leading to cell death.
3. Inhibition of Nucleic Acid Synthesis (DNA/RNA)
- Antibiotics: Fluoroquinolones, Rifamycins, Metronidazole.
- How it works: They stop the bacteria from making DNA or RNA, preventing reproduction and survival.
4. Inhibition of Protein Synthesis
- 30S Subunit Inhibitors: Aminoglycosides, Tetracyclines.
- 50S Subunit Inhibitors: Chloramphenicol, Macrolides, Clindamycin, Streptogramins
- How it works: These antibiotics block the bacterial ribosome, stopping protein production needed for growth and function.
5. Inhibition of Metabolic Pathways (Folate Synthesis)
- Antibiotics: Sulfonamides, Trimethoprim
- How it works: These drugs interfere with the production of folate, an essential nutrient for bacterial survival.
In Summary:
Antibiotics fight bacteria by:
- Breaking down their protective wall,
- Damaging their membrane,
- Stopping their genetic copying process,
- Blocking protein production, And interrupting their nutrient pathways,
- This multi-target strategy makes antibiotics highly effective in treating bacterial infections.
Mechanism of Cell Wall Synthesis Inhibitor
- Antibiotics (e.g., β-lactams) bind to the bacterial enzyme called transpeptidase.
- This blocks the transpeptidation process, which is essential for forming peptidoglycan, a major component of the bacterial cell wall.
- As a result, peptidoglycan synthesis is stopped, and the cell wall becomes weakened.
- This leads to leakage of cellular contents.
- The cell wall swells and eventually ruptures.
- Finally, this causes bacterial cell death.
The diagram on the right visually shows how failure of peptidoglycan
cross-linking leads to the breakdown of the cell wall — this is
referred to as the bactericidal effect.
Mechanism of Protein Synthesis Inhibitor
This image explains how bacterial protein synthesis is inhibited.
(Simple Explanation)
Protein Synthesis Inhibitor:
- Certain antibiotics such as Macrolide, Tetracycline, and Aminoglycoside act on the bacterial ribosome.
Binding to the 50S Ribosomal Subunit:
- These antibiotics bind to the 50S subunit of the bacterial ribosome.
Inhibits Protein Synthesis:
- As a result of this binding, the bacteria are unable to produce essential proteins.
Leads to inhibition of bacterial growth and reproduction:
- Since proteins are not produced, the bacteria stop growing and multiplying.
On the right side of the image, various parts of the ribosome are
shown, such as the A site, transferase site, mRNA template, and
tRNA, and their roles are illustrated.
- Bacteria also make their own food – they produce a type of food called protein which helps them survive and grow.
- These medicines (like macrolides and tetracyclines) enter the bacteria's "kitchen"!
- The bacteria's "kitchen" is a part of their body called the 50S ribosome.
- The medicines shut down this kitchen, so the bacteria can no longer make their food (proteins).
- Without food, the bacteria become weak and eventually die.
This is how medicine protects our body from illness.
Mechanism of Nucleic Acid (DNA & RNA) Synthesis Inhibitor
This image illustrates the mechanism of action of a class of
antibiotics called Quinolones, which are Nucleic Acid (DNA &
RNA) Synthesis Inhibitors.
Main Parts of the Image
Structure of Quinolones: On the left side, a chemical
structure is shown, which represents a quinolone antibiotic.
Mechanism of Action: Quinolones inhibit the
topoisomerase enzyme in bacteria.
On the right side, the image shows how quinolones affect bacterial
DNA:
- Quinolones inhibit an enzyme called topoisomerase in bacteria, which is essential for uncoiling DNA.
- Inhibition of this enzyme causes DNA damage and accumulation of Reactive Oxygen Species (ROS).
As a result, the bacteria die.
Contribution to Antibiotic Resistance:
- The use of quinolones leads to the selection of bacteria that are resistant to them.
- It can also induce resistance to other types of antibiotics.
- In summary, this image explains how quinolones destroy bacterial DNA and how they can contribute to the growing problem of antibiotic resistance.
Medicine Name: Moxifix
1. Moxifix blocks two important enzymes in bacteria-
- Topoisomerase II (DNA Gyrase)
- Topoisomerase IV
2. When these two enzymes are blocked, the bacteria cannot
produce their DNA.
3 Without making DNA, the bacteria cannot survive or grow.
4 As a result, Moxifix quickly kills the bacteria (Rapid
Bactericidal Activity).
In short:
*Moxifix stops bacterial DNA production, so the bacteria die
very quickly.
*The Magic Medicine That Kills Bacteria: Moxifix
*Imagine bacteria have a tiny copy machine that helps them make
copies of themselves.
*To run this machine, they need two buttons — one called DNA
Gyrase and the other called Topoisomerase IV.
*A medicine named Moxifix comes in and turns off both of these
buttons!
- As a result, the bacteria can no longer make copies of themselves.
- If they can’t copy themselves, they can’t grow.
- Eventually, they become weak and die.
This is how Moxifix quickly kills bacteria and keeps us healthy.
Mechanism of Cell Membrane Disruptor
This image explains the mechanism of action of Colistimethate
Sodium (Xylistin) or Colistin, an antibiotic belonging to the
Cell Membrane Disruptor class.
Main Content of the Image:
Colistimethate Sodium (Colistin): It is an antibiotic of
the polymyxin class.
Step-by-step Mechanism:
- Colistin binds to the lipopolysaccharides of the bacterial cell membrane.
- It then destabilizes the lipopolysaccharide structure.
- As a result, the cell membrane is disrupted.
Mode of Action in Short: Colistimethate Sodium
has a high binding affinity for lipopolysaccharides, which
leads to the disruption of the bacterial cell membrane and
ultimately kills the bacteria.
In summary, the image shows how Colistin destroys the
bacterial cell membrane and explains its mechanism in a
step-by-step manner.
Therapy-Resistance-Carrier Stage
Switch Therapy
- Switching from intravenous (IV) to Oral dosage form is called Switch Therapy.
- Example: Ceftriaxone (Trizon) —> Switching to —> Cefixime (Fix-A)
Antibiotic Resistance
Antibiotic resistance is the ability of a bacterial cell to
resist the harmful effect of an antibiotic.
Two types of bacterial resistance:
- Plasmid Resistance
- Enzymatic Resistance
Plasmid Resistance
Acquisition of antibiotic resistance occurs when genetic
material is taken up by the bacterial cell and either
incorporated into the chromosome, or, that is able to exist
in a stable form independent of the chromosome.
Such stable genetic elements that can not only exist but
that can replicate (reproduce) independently of the
chromosome, are known as plasmids.
If the genetic information encoded (fixed) by a plasmid
leads to resistance against a particular antibiotic, this
plasmid is known as a resistance plasmid. Example: MRSA.
Enzymatic Resistance
Enzymatic inactivation of the antibiotic is called enzymatic
resistance.
The best known example of enzymatic inactivation of
antibiotics is that of the B-lactamases.
These enzymes render B-lactam antibiotics inactive by
cleaving the lactam ring of susceptible antibiotics via an
irreversible hydroxylation of the amide bond.
b-lactamases are a common resistance mechanism among
Gram-positive and Gram-negative organisms, both aerobic and
anaerobic.
Cross-resistance
Microorganisms resistant to one drug may also show resistance
to a second drug that has a similar mode of action or with
similar structure even without being exposed to the second
drug. Such a phenomenon is called cross-resistance.
Carrier Stage
It is a condition where a person harbors a pathogenic organism
but does not show any symptoms of disease.
After suffering from typhoid many people become carriers of
typhoid and spread the disease.
That is why typhoid should receive sufficient treatment to
eradicate the typhoid bacilli.
Methicillin Resistant Staphylococcus aureus
MRSA stands for Methicillin-Resistant Staphylococcus aureus, a
type of bacteria that is resistant to several antibiotics.
These strains are resistant to penicillin, amoxicillin and
beta lactam agents including cephalosporin.
Delafloxacin is effective against MRSA.
Post-Antibiotic Effect
PAE is the effect of the antibiotic during the period between
removal of the antibiotic and the complete recovery of normal
bacterial growth.
- PAE = T - C
PAE (Post-antibiotic effect): Time required for culture to
return to logarithmic growth.
T = time required for the viable count to increase 10X above
the count at the time the drug is removed from the culture.
C = time required for the count to increase 10X in an
untreated culture.
Properties of an Ideal Antibiotic
The properties of an ideal antibiotic are divided on the
basis of 4 (four) factors:
- Efficacy: The ability to produce an effect.
- Safety: The level of side effects / adverse effects of a drug.
- Convenience: The flexibility and comfort to take the medicine.
- Cost: How much is the expense of treatment with the medicine.
1. Efficacy
- Should be broad spectrum, which means able to kill or inhibit both gram-positive and gram-negative pathogens.
- Should be bactericidal rather than bacteriostatic.
- Absorption and distribution of the drug should be rapid.
- Should be excreted through urine in an active unchanged form to be effective in UTI.
- MIC against culprit pathogens must be lower than that of Peak plasma concentration (Cmax).
- Microorganisms should not be able to develop resistance.
- Absorption should be independent of the presence of food in the stomach.
- Should have antibacterial efficacy that is not reduced by body fluids, exudates, plasma proteins or tissue enzymes.
- Achieve and maintain bactericidal levels in blood, tissue and body fluids. I.e. CSF.
- Should not be contraindicated with other drugs.
2. Safety
- Should be suitable for all age groups and sex.
- Bacterial resistance in target pathogens should be no or very low.
- Should be safe for pregnant or lactating mothers.
- Side effects of the drug should be as low as possible.
3. Convenience
- Should be long acting rather than short acting.
- Should not have unpalatable after taste of the drug.
- Should be available both in oral and parenteral form.
- Should possess a short duration of therapy.
4. Cost
- Drugs should be cost effective.
Minimum inhibitory and bacterial concentration
MIC (Minimum Inhibitory Concentration)
Minimum Inhibitory Concentration is the lowest concentration
of an antibiotic in the plasma that inhibits the growth of
target pathogens.
Example: MICg0S (µg/ml) of Ciprofloxacin against E.coli
is 0.03, which means that 0.03 µg/ml concentration of
ciprofloxacin is effective to inhibit 90% growth of the E.
coli.
MBC (Minimum Bactericidal Concentration)
Minimum Bactericidal Concentration is the lowest drug
concentration in the plasma that kills the target pathogen.
Example: The MBC of Ciprofloxacin against E.coli is
0.004 (mg/l), which means that 0.004 mg/l concentration of
ciprofloxacin is effective to kill 99.9% of the E. coli.
Penicillin antibiotics explain in details
Classification of Penicillin
A. Natural Penicillin: Phenoxy methyl Penicillin (Pen-V)
B. Semisynthetic Penicillin
- Beta lactamase resistant penicillin : Flucloxacillin
- Non Beta lactamase resistant penicillin : Amoxicillin
Strengths of Penicillin
- Broad spectrum of activity
- Higher safety profile in children and pregnant mothers
- Lesser side effects
- Convenient dosage schedule
Weakness of Semisynthetic Penicillin
- Penicillin is inactivated by beta lactamases and are therefore not effective against most Staphylococcal infections.
- Inactive against Pseudomonas aeruginosa.
- Cross-allergenicity exists between all types of penicillins.
- Amoxicillin is not useful in the treatment of Shigella and Salmonella infections.
- Hypersensitivity reactions.
Cephalosporins generations antibiotic explain in details
Cephalosporins are semisynthetic antibiotics that are
derived from fungi cephalosporium (Cephalosporium
acremonium).
Side chain modifications to the nucleus of beta
lactam ring offers:
- An improved spectrum of antibacterial activity.
- Pharmacokinetic advantages.
Strength of Cephalosporins
- Broad spectrum of antimicrobial activity.
- Increasing resistance to destruction by beta-lactamases.
- Outstanding safety profile in children and pregnant women.
- Very good tissue penetration.
- Lesser side effects than other antibiotics.
- Convenient dosage schedule.
- Both oral and parenteral dosage forms are available.
- Less allergic than that of penicillin.
Weakness of Cephalosporins
- Inadequate cerebrospinal fluid penetration of 1 ^ (st) and 2 ^ (nd) generation cephalosporins.
- Limited activity against enterococci and pseudomonas.
- Gram positive coverage diminishes with each successive generation of cephalosporins.
- Diarrhoea has more common side effects with 2 ^ (nd) and 3 ^ (rd) generation.
- Patients who have a history of penicillin allergy should avoid cephalosporins.
Difference between Generation of Cephalosporins
| Generation of Cephalosporins | Activity against gram Positive organisms | Activity against grame negativelorganisms |
|---|---|---|
| 1st generation | ++++ | ++ |
| 2nd generation | +++ | +++ |
| 3rd generation | ++ | ++++ |
| 4th generation | +++ | ++++ |
Here,
- Higher coverage = ++++
- Moderate coverage = +++
- Lesser coverage = ++
First Generation Cephalosporins
Strengths:
- Good activity against staphylococci, streptococci, pneumococci, some anaerobic cocci.
- Prophylaxis of wound infections following surgery, SSTI.
- Used as Alternative to penicillin in penicillin-allergic individuals.
Weakness:
- Weaker gram negative coverage.
Second Generation Cephalosporins
Strengths:
- Extended gram negative coverage against Klebsiella, Proteus, Haemophilus, E.coli and Moraxella.
- Used to treat abdominal and gynecological infections, UTI & Lower RTI.
Weaknesses:
- Poor activity against P. aeruginosa.
- Not active against Salmonella typhi, atypical pathogen and anaerobic bacteria.
Third Generation Cephalosporins
Strengths:
- Extended activity against gram negative bacilli, particularly enterobacteriaceae & H. influenzae.
- Few side effects and less allergenic than penicillin.
- Important drugs for treating bacterial meningitis.
- Ceftazidime is active against P. aeruginosa and safe for neonates from day one.
- Can be used in renal dysfunction without any dose adjustment.
- Ceftriaxone is the safest treatment option for paediatric patients in typhoid/enteric fever.
Weaknesses:
- Reduced activity against S. aureus.
- More resistant to non-Staphylococcus ẞ-lactamase.
Fourth Generation Cephalosporins
Strengths:
- Increased gram positive cocci activity against S. viridians and penicillin resistant pneumococcus.
- More effective against Enterobacteriaceae.
- Improved resistance to beta lactamases compared to the third generation.
Weaknesses:
- Not indicated in children.
- Not active against Klebsiella.
- Need to combine with aminoglycoside to cover P. aeruginosa.
Macrolides generations antibiotic explain in details
Macrolides are a large group of antimicrobials derived from
Actinomycetes (soil bacteria) or semi synthetic derivatives of
them.
Macrolides are characterized chemically by a large
"macrocyclic" ring structure.
The structural differences in Macrolides make them ideal
alternatives to penicillin in patients who have penicillin
allergies.
Pseudomonas, E.coli and Klebsiella strains are resistant to
erythromycin.
Pneumococci that are resistant to penicillin are resistant to
macrolides.
Erythromycin does interact adversely with drugs oxidized by
Cytochrome p-450 eg, Simvastatin, Theophylline.
Macrolides Generations
- First generation : Erythromycin (Erocin)
- Second generation : Azithromycin (Azin), Clarithromycin (Claricin), Roxithromycin
- Third generation : Telithromycin, Cethromycin and Solithromycin.
Advantages of Azithromycin over Erythromycin
The addition of Nitrogen at position 9a of the lactone
ring gives azithromycin:
- Decrease GI side effects
- Increase Spectrum of activity
- Fewer drug interactions
- Less frequent dosing (increase compliance)
- Better tissue penetration
Fluoroquinolone generations antibiotic explain in details
The fluoroquinolones are a series of synthetic
antibacterial agents that are used in the treatment of
a variety of bacterial infections. All
fluoroquinolones accumulate within bacteria very
rapidly.
Classification:
- First generation : Nalidixic acid (Naligram)
- Second generation : Ciprofloxacin (Cipro-A)
- Third generation : Levofloxacin (Leo)
- Fourth generation : Moxifloxacin (Moxifix), Delafloxacin (Delaflox).
Strengths of Fluoroquinolones
- Potent activity against gram negative pathogens.
- Long acting than penicillin / erythromycin / cephalosporins.
- Suitable for treatment of bacterial infections due to multidrug resistant organisms.
- Excellent activity against S. typhi and all strains of Enterobacteriaceae.
- Patients who are allergic to the penicillin, cephalosporins, sulfonamides, erythromycin can shift to fluoroquinolones.
- Able to be active against plasmid mediated resistance of bacteria in case of MRSA.
- Superb synergistic effect with metronidazole.
Weakness of Fluoroquinolones
Fluoroquinolones are not recommended for children, pregnant
or breastfeeding mothers due to bone development problems.
Not useful against infections caused by anaerobes.
Fluoroquinolones may cause phototoxicity from exposure to
sunlight.
Bioavailability of all quinolones is impaired by di and
trivalent cations in stomach (eg. Al+++, Ca++, Mg++, Fe++,
Zn++, as in vitamins with zinc or iron or in antacids).
First Generation Fluoroquinolones
Strengths:
- Activity against gram negative organisms.
Weaknesses:
- More frequent dosing.
- Susceptible more to development of bacterial resistance.
- Minimum serum level is achieved, so use of drugs has been restricted in UTI.
Second Generation Fluoroquinolones
Strength:
- Very active against aerobic gram-negative bacilli.
- Has excellent oral bioavailability.
- Excellent activity against S.typhi and all strains of Enterobacteriaceae.
- Able to be active against plasmid mediated resistance of bacteria in case of MRSA.
- Increase gram negative, gram positive and atypical pathogen coverage.
- Because of good penetration into the bone, orally administered ciprofloxacin is a useful alternative to parenterally administered antibiotics for osteomyelitis.
Second Generation Fluoroquinolones
Limitations:
- Is not active against anaerobes.
- Has only limited activity against streptococci and staphylococci.
- S. pneumoniae is frequently resistant to this class.
Third Generation Fluoroquinolones
Strength:
- Expanded activity against gram-positive organisms, particularly penicillin-sensitive and penicillin-resistant S. pneumoniae, and atypical pathogens such as Mycoplasma pneumoniae and Chlamydia pneumoniae.
- Treatment of community-acquired pneumonia, acute sinusitis and acute exacerbations of chronic bronchitis - primary FDA-labeled indications.
Limitation:
- Less active against P. aeruginosa species
- Significant risk of phototoxicity.
Fourth Generation Fluoroquinolones
Strengths:
- Significant antimicrobial activity against anaerobes while maintaining the gram-positive and gram-negative activity of the third-generation quinolones.
- Retains activity against Pseudomonas species comparable to that of ciprofloxacin.
- Originally labeled by the FDA for the treatment of a wide spectrum of infectious diseases.
Aminoglycosides antibiotics explain in details
Aminoglycosides are a group of antibiotics that are used to
treat certain bacterial infections.
This group of antibiotics includes:
- Amikacin
- Gentamicin
- Kanamycin
- Neomycin
- Streptomycin
- Tobramycin
Aminoglycosides antibiotics Mechanism of action
- Aminoglycoside attaches to a bacterial cell wall and is drawn into the cell via channels made up of the protein, porin.
- Once inside the cell, the aminoglycoside attaches to the cell's ribosomes.
- This attachment either shuts down protein production or causes the cell to produce abnormal, ineffective proteins.
- And the bacterial cell eventually destroys.
(Aminoglycoside + Beta lactam) combination
When Aminoglycocides are given with beta lactam antibiotics,
it gives synergistic effects in case of all common
gram-positive and gram-negative infections.
Beta-lactamase disrupts the integrity of the bacteria cell
wall, making it more porous. The increased porosity allows
more of the aminoglycoside into the bacteria cell.
Strength of Aminoglycosides
- Amikacin - Least susceptible to resistance.
- Aminoglycosides are often included in combination antibiotic regimens for polymicrobial infections and for prophylaxis in surgery.
- Active against Pseudomonas aeruginosa klebsiella pneumoniae, enterobacteriaceae, serratia and proteus species.
- Reserved for serious infection due to aerobic gram negative bacilli.
Weakness of Aminoglycosides
- Ototoxicity
- Nephrotoxicity
- Poor crossing of blood brain barrier
- Narrow therapeutic range - not greater than 2mcg/ml
- Not active against Streptococci, Pneumococci, and Enterococci
Tetracycline antibiotics explain in details
The antibiotic effect of tetracycline is based on an
inhibition of the ribosomal protein synthesis of the
bacteria. The tetracycline ties up at a special
connection place of the ribosome. Thus the complete
formation of the protein chain is interrupted and
prevents the reproduction process of the bacteria.
Examples:
- Tetracycline
- Oxytetracycline
- Doxycycline (Doxy-A)
- Minocycline
Advantages of Doxycycline over Tetracycline
- Improved admission in the intestine than tetracycline.
- Gastro-intestinal side effects are reduced than tetracycline.
- Increased compatibility than tetracycline.
Weakness of Tetracyclines
- Tetracyclines may cause yellowish discoloration of the teeth.
- Many streptococcus and pneumococcus strains have become resistant to tetracyclines.
- Most S. aureus, most bacteroides, some mycoplasma, and all Pseudomonas aeruginosa strains are resistant.
- Tetracyclines are contraindicated in pregnancy because of fetal bone growth inhibition.
Cotrimoxazole
Cotrimoxazole is the combination of sulfamethoxazole and
trimethoprim. These drugs have a wide range of antimicrobial
activity against gram-positive and gram-negative bacteria by
providing synergistic action.
This image explains the step-by-step mechanism of action of
the antibiotic combination Trimethoprim-Sulfamethoxazole.
Step-by-step process:
1. PABA (Para-Aminobenzoic Acid) is a component used by
bacteria to make folic acid.
2. Sulfonamides (e.g., Sulfamethoxazole)
- Inhibit the enzyme Tetrahydro Pteroic acid synthase, preventing the formation of;
3. Dihydrofolic acid.
- This blocks the first step of folic acid synthesis.
4. Trimethoprim
- Inhibits the enzyme Dihydrofolate reductase, which converts Dihydrofolic acid into Tetrahydrofolic acid.
- This blocks the next step needed for purine and DNA synthesis.
Summary:
- Sulfamethoxazole blocks the first step in folic acid production.
- Trimethoprim blocks the final step in the conversion.
- As a result, DNA synthesis is disrupted, and the bacteria cannot grow or survive.
- This combination is very effective in stopping bacterial growth.
Mechanism of action
- Sulfamethoxazole and trimethoprim both act by inhibiting the synthesis of folic acid.
- Sulfonamide inhibits the formation of dihydrofolic acid from PABA (Para Amino Benzoic Acid).
- Trimethoprim inhibits the formation of tetrahydrofolic acid from dihydrofolic acid.
- Thus they are used in combination to produce great synergistic effects.
Meropenem antibiotics
Meropenem is an antibiotic of Carbapenem Group.
Meropenem is used after initial therapy when
cephalosporins or penicillins have been ineffective.
Meropenem is useful for the treatment of serious
hospital-acquired or mixed infections in which
aerobic and anaerobic gram-negative bacilli plus S.
aureus might be involved.
Indications
- Intra-abdominal infections.
- Septicaemia.
- Empiric treatment, including initial monotherapy, for presumed bacterial infections in host compromised, neutropenic patients.
- Meningitis.
- Lower RTI.
- Gynecological infections, including postpartum infections.
- Complicated UTI.
Classification Chart With ACME Brand and Generic
Since I worked at
Acme Laboratories Limited, I am providing the names and generic names of Acme
Laboratories Limited's antibiotic drugs as examples. You
should memorize the antibiotic drugs of the pharmaceutical
company in which you will work.
Classification Chart of ACME's Antibiotic
Therapeutic Class - Antibiotic:
1. Beta-lactam
- Penicillin
- Cephalosporin
- Carbapenem
2. Macrolides
3. Fluoroquinolones
4. Tetracycline
5. Polypeptides
Details:
1. Beta-lactam
Penicillin: Cloxacillin (A-Clox), Flucloxacillin
(A-Flox), Amoxicillin (Moxilin)
Cephalosporin:
- 1st generation: Cephradine (Sefril), Cefadroxil (Twicef)
- 2nd generation: Cefaclor (Alcior), Cefuroxime (Famicef)
- 3rd generation (Oral): Cefixime (Fix-A), Cefpodoxime (CP), Ceftibuten (Logibec)
- 3rd generation (Parenteral): Ceftriaxone (Trizon), Ceftazidime (Trizidim)
- 4th generation: Cefepime (Superpime)
Carbapenem: Meropenem (Fulspec)
Macrolides
- Azithromycin (Azin), Clarithromycin (Claricin), Erythromycin (Erocin)
Fluoroquinolones
- 1st generation: Nalidixic acid (Naligram)
- 2nd generation: Ciprofloxacin (Cipro-A)
- 3rd generation: Levofloxacin (Leo)
- 4th Generation: Moxifloxacin (Moxifix), Delafloxacin (Delaflox)
Tetracycline
- Tetracycline (A-Tetra), Doxycycline (Doxy-A)
Polypeptides
- Colistimethate Sodium (Xylistin)
Indication Chart of Antibiotic Generic
URTI: Upper Respiratory Tract Infection
- Erythromycin
- Cefadroxil
LRTI: Lower Respiratory Tract Infection
- Amoxicillin
- Cefepime
- Ceftazidime
- Delafloxacin
- Colistimethate Sodium
UTI: Urinary Tract Infection
- Cefuroxime
- Cefuroxime+Clavulanic Acid
- Cefepime
- Ceftazidime
Both URTI & LRTI:
- Cefradine
- Cefuroxime
- Cefuroxime+Clavulanic Acid
- Cefaclor
- Ceftibuten
- Cefixime
- Cefpodoxime Proxetil
- Azithromycin
- Clarithromycin
- Tetracycline
- Doxycycline
SSSI: Skin and Soft Structure Infection
- Cloxacillin
- Flucoxacillin
- Cefradine
- Cefadroxil
- Cefuroxime
- Ceftriaxone
- Ceftazidime
- Cefpodoxime Proxetil
- Azithromycin
- Erythromycin
- Delafloxacin
Typhoid:
- Cefuroxime+Clavulanic Acid
- Ceftriaxone
- Cefixime
- Azithromycin
Diarrhoea:
- Ciprofloxacin
- Azithromycin
- Tetracycline
- Doxycycline
STD: Sexually Transmitted Disease
- Cefixime
- Azithromycin
- Tetracycline
- Doxycycline
Septicemia:
- Cefepime
- Ceftazidime
- Meropenem
CNS Infections: Central Nervous System Infections
- Ceftazidime
- Meropenem
- Ceftriaxone
Intra abdominal Infections:
- Ceftazidime
- Meropenem
- Cefepime
Oral & Parenteral Antibiotic Brands of ACME Laboratories Ltd.
Only Oral:
- Cephalosporin Antibiotic: Sefril, Twicef, Famiclav, Alclor, Logibac, Fix-A, CP.
- Non Cephalosporin Antibiotic: A-Clox, Moxilin, A-Tetra, Doxy-A, Azin, Erocin, Claricin, Leo.
Only Parenteral: Trizon, Superpime, Trizidim,
Fulspec, Delaflox, Xylistin.
Both Oral & Parenteral: Famicef, A-Flox,
Cipro-A, Moxifix.
FAQs about basic information about antibiotics and generic drugs
1. Do antibiotics work against viruses?
No, antibiotics do not work against viruses like the
flu, cold, or COVID-19. Antibiotics only treat
bacterial infections.
2. Can we stop taking antibiotics once I feel
better?
No. We should always complete the full course as
prescribed by a doctor to make sure all bacteria are
fully removed.
3. What happens if antibiotics are overused?
Overuse or misuse can lead to antibiotic resistance,
where bacteria stop responding to the medicine.
4. Are there any side effects of antibiotics?
Yes. Common side effects include stomach upset,
diarrhea, allergic reactions, and yeast infections.
5. What is a broad-spectrum antibiotic?
It is an antibiotic that works against a wide variety of
bacteria, both gram-positive and gram-negative.
6. What are generic antibiotics?
Generic antibiotics have the same active ingredient,
strength, and effect as brand-name drugs but are often
more affordable.
Conclusion
You’ve just explored the essential basics of antibiotics
and generics—two powerful pillars of the pharma world.
For any future Medical Promotion Officer (MPO), this
knowledge isn't optional—it’s necessary. By learning the
basic information about antibiotics and generic drugs,
you're already one step ahead. This article aimed to
make things simple and practical. Take this
understanding forward as you move closer to your
pharmaceutical goals.