CNS disease basic and product details | MPO training 22
If you're starting your journey as a Medical Promotion Officer (MPO), you’ll
need to understand CNS diseases and how related products work. This content
helps you explore the CNS disease basic and product details in a way that's
simple and clear. You’ll discover essential drug names, usage patterns, and
core medical facts that you need every day in the field.
Whether you're preparing for a job or already working, this can guide you. You
won’t get overwhelmed - every detail is made easier for you. Let this be your
go-to learning tool for real success in the pharma world.
Table of contents: CNS disease basic and product details
Check out what you will learn from this article-
CNS disease basic
CNS disease basic and product details include common brain and nerve
conditions like epilepsy, depression, and Parkinson’s disease. These
diseases often require medications such as carbamazepine, fluoxetine, and
levodopa. As a Medical Promotion Officer (MPO), you must know both the
generic and branded names, their indications, and key benefits.
This helps you communicate clearly with doctors and pharmacists. The right
knowledge gives you confidence in the field. This quick guide makes it
easier for you to remember and apply these details in your daily work.
What is the central nervous system (CNS)?
The central nervous system (CNS) includes the brain and spinal cord. It
controls how your body functions, thinks, moves, and feels.
What are some common CNS diseases?
Common CNS diseases include epilepsy, Parkinson’s disease, multiple
sclerosis, depression, anxiety, and Alzheimer’s disease
So let us first learn about CNS disease basics and then we will learn about
generic names and brand name products.
Neurological Disorder
There is ample evidence that pinpoints neurological disorders as one of the
greatest threats to public health. There are several gaps in understanding
the many issues related to neurological disorders, but we already know
enough about their nature and treatment to be able to shape effective policy
responses to some of the most prevalent among them.
Anxiety Disorder
Anxiety disorders are a group of mental disorders characterized by
significant feelings of anxiety and fear. Anxiety is a worry about future
events, while fear is a reaction to current events.
Symptoms of Anxiety
The image visually presents common signs of anxiety-
- Excessive anxiety and worry
- Fatigue
- Restlessness
- Increased muscle aches or soreness
- Impaired concentration
- Irritability
- Difficulty sleeping
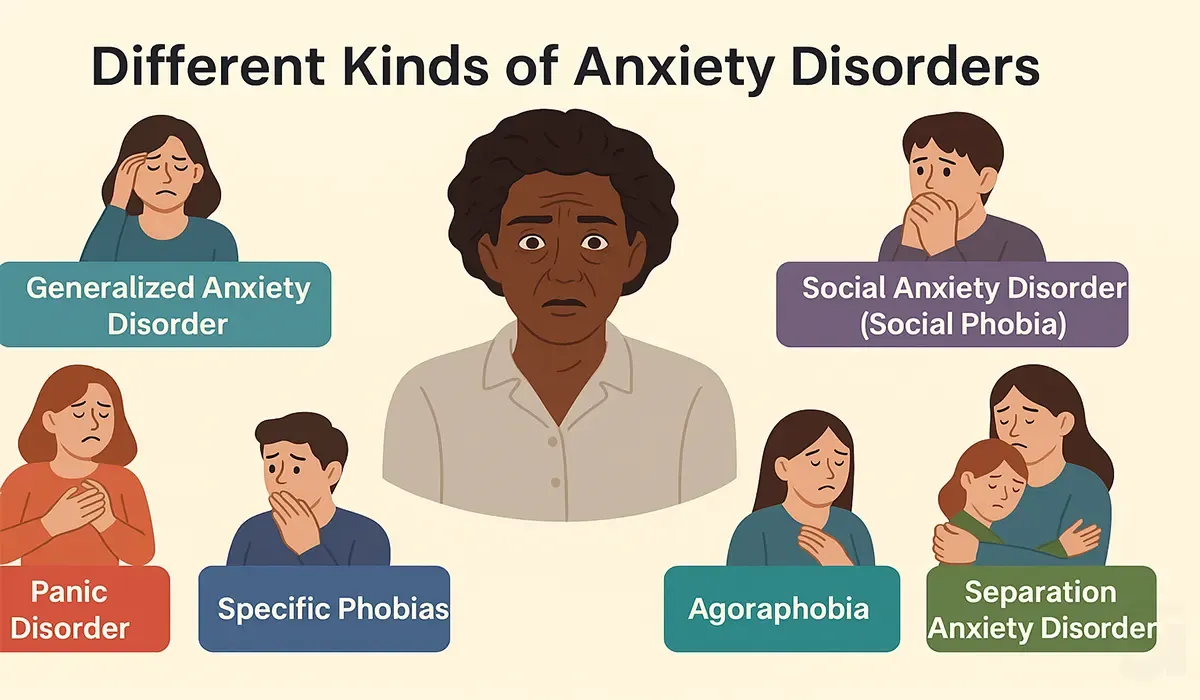
Different Kinds of Anxiety Disorders
Generalized anxiety disorder (GAD)
Generalized anxiety disorder (GAD) is a common disorder, characterized
by long-lasting anxiety which is not focused on any one object or
situation. Those suffering from generalized anxiety disorder experience
non-specific persistent fear and worry, and become overly concerned with
everyday matters.
Phobias
The single largest category of anxiety disorders is that of specific
phobias which includes all cases in which fear and anxiety are
triggered by a specific stimulus or situation.
Common phobias are flying, blood, water, highway driving, and tunnels.
When people are exposed to their phobia, they may experience
trembling, shortness of breath, or rapid heartbeat. People understand
that their fear is not proportional to the actual potential danger but
still are overwhelmed by it.
Panic Disorder
With panic disorder, a person has brief attacks of intense terror and
apprehension, often marked by trembling, shaking, confusion,
dizziness, nausea, and/or difficulty breathing.
These panic attacks, defined by the APA as fear or discomfort that
abruptly arises and peaks in less than ten minutes, can last for
several hours. Attacks can be triggered by stress, irrational
thoughts, general fear or fear of the unknown, or even exercise.
Obsessive Compulsive Disorder
It is a condition where the person has obsessions (distressing,
persistent, and intrusive thoughts or images) and compulsions (urges
to repeatedly perform specific acts or rituals), that are not caused
by drugs or physical disorder, and which cause distress dysfunction.
Depression
Depression is a mood disorder that causes a persistent feeling of
sadness and loss of interest and can interfere with your daily
functioning.
Symptoms of Depression
The common signs of depression are as follows:
- Low mood – Feeling sad or down most of the time
- Changes in appetite – Eating significantly more or less than usual
- Sleep disturbance – Trouble sleeping or sleeping too much
- Agitation – Feeling restless or easily irritated
- Fatigue – Persistent tiredness or lack of energy
- Difficulty concentrating – Trouble focusing or making decisions
These symptoms, if experienced over a prolonged period, may indicate
depression, and it's advisable to seek professional help if they
persist.
Insomnia
Insomnia is a sleep disorder in which you have trouble falling and/or
staying asleep.
Agitation
An emotional state of excitement or restlessness.
Anorexia
Anorexia nervosa, often referred to simply as anorexia, is an eating
disorder, orexia, characterized by low weight, food restriction, fear of
gaining weight and a strong desire to be thin.
Mixed Anxiety And Depression Disorder (MADD)
When symptoms of anxiety and depression are both present, but neither is
clearly predominant and neither type of symptom is present to the extent
that justifies a diagnosis if considered separately.
Causes Of MADD:
It shows a person surrounded by thought bubbles, each representing a
potential cause of MADD.
Here are the causes listed in the image:
- Early traumatic event – Experiencing trauma early in life.
- Parenting style – Negative or overly strict parenting can contribute.
- Isolated upbringing – Growing up in isolation or without social interaction.
- Brain structure – Certain brain structures may influence mood and anxiety.
- Societal expectations – Pressure to meet societal standards or norms.
- Genetics – Family history or inherited traits.
- Observing others with SAD (Social Anxiety Disorder) – Learning behaviors from people with anxiety.
The image illustrates that MADD can have multiple causes, including both
environmental and biological factors.
Psychosomatic Disorder
Psychosomatic disorder, also called Psychophysiological Disorder is a
condition in which psychological stresses adversely affect physiological
(somatic) functioning to the point of distress.
Neuropathic Pain
Neuropathic pain is pain caused by damage or disease affecting the
somatosensory nervous system.
Peripheral Neuropathy
Peripheral neuropathy, often shortened to neuropathy, is a general term
describing disease affecting the peripheral nerves, meaning nerves
beyond the brain and spinal cord.
This image explains in a simple way the types of symptoms that may occur
when different types of nerves in the human body are damaged. It shows
the signs of damage to three types of nerves separately.
* Sensory Nerve Damage: These nerves are responsible for our
sense of feeling. When damaged, the following symptoms may occur:
- Unusual sensations
- Pain from light touch
- Burning sensations
- Numbness
- Tingling or pins and needles
- Balance problems
* Motor Nerve Damage: These nerves control our muscle movements.
When damaged, it may cause:
- Muscle cramping
- Delayed response due to reflex problems
* Autonomic Nerve Damage: These nerves regulate automatic
functions such as sweating, digestion, and blood pressure. Damage to
these nerves may lead to:
- Excess sweating
- Heat intolerance
- Feeling full quickly after eating
- Impotence
- Dizziness or fainting when standing up (Orthostatic hypotension)
This image is designed to help you easily understand the types and
symptoms of nerve damage.
Fibromyalgia
Fibromyalgia is a disorder characterized by widespread musculoskeletal
pain accompanied by fatigue, sleep, memory and mood issues.
Researchers believe that fibromyalgia amplifies painful sensations by
affecting the way your brain and spinal cord process painful and
painless signals.
Seizure And Epilepsy
A seizure is a sudden, uncontrolled electrical disturbance in the
brain. It can cause changes in your behavior, movements or feelings,
and in levels of consciousness.
Epilepsy is a chronic disorder that causes unprovoked, recurrent
seizures.
Convulsion
A convulsion is a medical condition where body muscles contract and
relax rapidly and repeatedly, resulting in uncontrolled actions of the
body.
Migraine
Migraine is a neurological condition that can cause multiple symptoms.
It's frequently characterized by intense, debilitating headaches.
Symptoms may include nausea, vomiting, difficulty speaking, numbness
or tingling, and sensitivity to light and sound. Migraines often run
in families and affect all ages.
Parkinson's Disease
It is a long-term degenerative disorder of the central nervous system
that mainly affects the motor system. Parkinson's symptoms usually
begin gradually and get worse over time.
Symptoms of Parkinson’s Disease:
- Parkinsonian gait – A characteristic way of walking with a stooped posture and small, shuffling steps.
- Slowed movement (bradykinesia) – Movements become slower over time.
- Reduced arm swing – The natural swinging motion of the arms while walking is decreased.
- Rigidity – Stiffness in the limbs or trunk.
- Freezing – Sudden, temporary inability to move.
- Mask-like face – Reduced facial expressions, making the face look emotionless.
- Asymmetric resting tremor – Shaking, usually starting on one side of the body, especially noticeable at rest.
- Postural instability – Difficulty maintaining balance, leading to a tendency to fall.
- Shuffling steps – Taking short, dragging steps while walking.
This condition affects daily life and requires medical attention and
ongoing management.
Drugs Acting on CNS
There are mainly two groups:
- CNS depressants.
- CNS Stimulants.
CNS Depressants
CNS Depressants can be classified into:
- Sedative-Hypnotics able to cause sedation (with concomitant relief of anxiety) or to encourage sleep (hypnosis).
- Anxiolytic drugs - reduces anxiety.
- Anticonvulsants - used for the treatment of epileptic seizures.
- Antipsychotics - primarily used to manage psychosis.
- Antidepressants- medications that can help relieve symptoms of depression.
- Skeletal muscle relaxant properties.
CNS Stimulants
Directly acting on CNS:
- Cortical- Caffeine, Amphetamine
- Medullary- Adrenaline
- Spinal-Strychnine
Reflexly acting on CNS:
- Nicotine, Lobetine
Action Potential
Action potentials are nerve signals. Neurons generate and
conduct these signals along their processes in order to transmit
them to the target tissues. Only neurons and muscle cells are
capable of generating an action potential.
This image illustrates the process of an Action Potential,
which is the generation of an electrical signal in a nerve
cell (neuron).
A step-by-step explanation is given below:
Step 1: Stimulus
- An external stimulus (such as touch, pressure, etc.) excites the neuron.
- At this point, the voltage inside the cell begins to rise gradually.
- If the stimulus is not strong enough, it cannot reach the threshold level — this is known as a Failed initiation.
Step 2: Threshold Crossing and Na⁺ (Sodium) Influx
- If the stimulus is strong enough and crosses the threshold level (usually around -55mV), an Action Potential is triggered.
- At this stage, sodium ions (Na⁺) enter the cell, causing a rapid increase in voltage.
Step 3: Action Potential (Active Phase)
- As sodium ions enter, the internal voltage of the cell rises up to about +40mV.
- This is known as the Action Potential, the active electrical signal that propagates along the nerve.
Step 4: Repolarization and Hyperpolarization
- Now, potassium ions (K⁺) begin to exit the cell.
- As a result, the voltage starts to fall again — this is called Repolarization.
- Sometimes the voltage drops below the resting level of -70mV — this is called Hyperpolarization.
Step 5: Resting State
- Finally, the voltage returns to the normal Resting State (about -70mV).
- The cell is now ready for the next action potential.
Summary: This graph shows how a neuron generates an
electrical signal in response to an external stimulus, how the
signal propagates, and how the neuron returns to its resting
state. This is the fundamental mechanism of nerve signal
transmission.
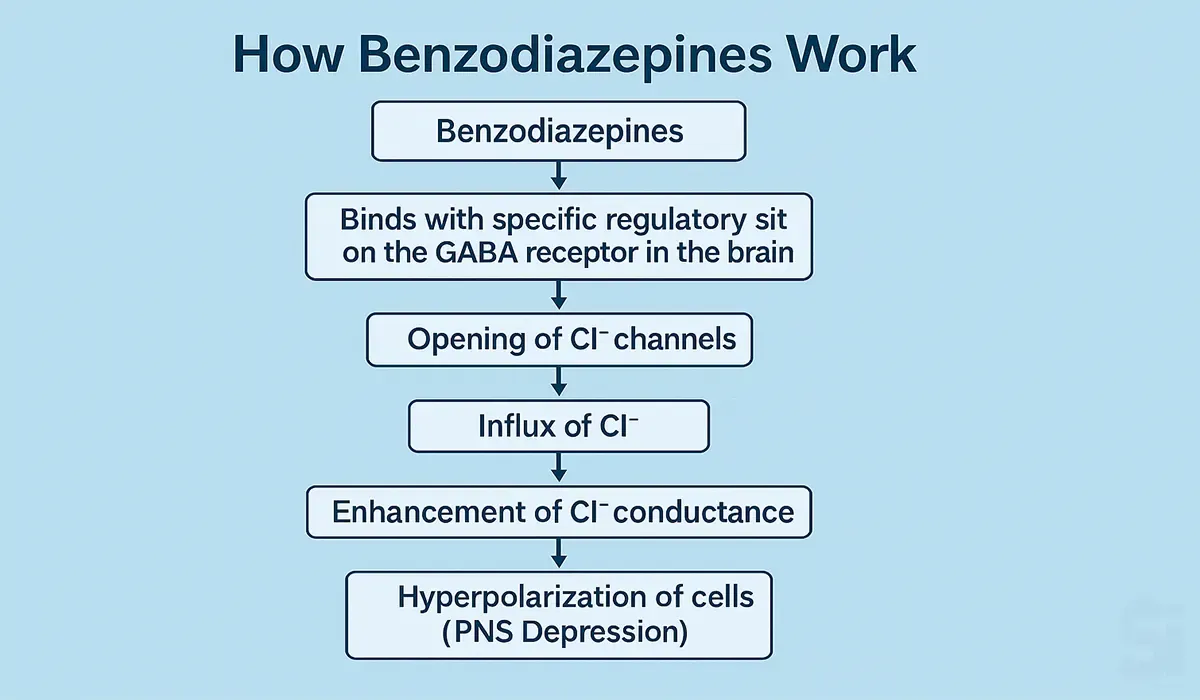
How Benzodiazepines Works
This image explains how Benzodiazepines work in our brain.
Main Idea: In our brain, there is a chemical called
GABA (Gamma-Aminobutyric Acid). It is a calming
neurotransmitter – it helps keep our nerves relaxed and
reduces excessive excitement.
How do Benzodiazepines work?
The image shows a GABA receptor complex, which is like a gate
or channel that controls the flow of certain chemicals in and
out of the nerve cell.
When GABA binds to its specific receptor, it allows Cl⁻
(chloride ions) to enter the cell. This flow of chloride ions
calms the nerve cell.
Benzodiazepines enhance the effect of GABA. That means when
GABA is working, benzodiazepines make its calming effect even
stronger, resulting in a greater feeling of relaxation.
Other drugs like Zolpidem, Flumazenil, and Barbiturates also
act on this receptor in different ways, but benzodiazepines
are the most commonly used for treating sleep disorders,
anxiety, and seizures.
In Summary: Benzodiazepines strengthen the action of
GABA, helping calm the brain and reduce anxiety or panic.
Step-by-Step Action of Benzodiazepines on GABA Receptors
Step-by-step Explanation:
1. Benzodiazepines bind to the GABA receptor in the brain.
- These receptors are proteins found on nerve cells that regulate the activity of the central nervous system (CNS).
2. Binding enhances the effect of GABA, causing Cl⁻
(chloride) channels to open.
- This allows chloride ions to flow into the neuron.
3. Influx of Cl⁻ (chloride ions) into the neuron occurs.
- The inside of the cell becomes more negative.
4. This increases chloride conductance within the cell.
- It stabilizes the neuron and makes it less responsive to stimulation.
5. Hyperpolarization of the neuron occurs.
- This makes the inside of the neuron even more negative than at rest, reducing the chance of firing an action potential.
6. Reduced ability to generate an action potential.
- Since neurons are less excitable, they are less likely to transmit signals.
7. Overall effect: Central Nervous System (CNS) depression.
- This leads to a calming effect on the brain, known as postsynaptic inhibition.
In summary: Benzodiazepines bind to GABA receptors in
the brain, allowing chloride ions (Cl⁻) to enter nerve
cells. This makes the cells more stable and less excitable.
As a result, symptoms like anxiety, overexcitement, or sleep
disturbances are reduced.
How Selective serotonin reuptake inhibitors (SSRI) Works
This image shows how SSRIs (Selective Serotonin Reuptake
Inhibitors) work.
Main Point: In our brain, there is a chemical called
serotonin, which helps keep our mood stable and makes us
feel good. This serotonin flows through a small gap between
two nerve cells called the synapse.
How do SSRIs work?
- Serotonin is normally released from the presynaptic cell and moves to the postsynaptic cell.
- After that, some of the serotonin goes back into the presynaptic cell — this process is called reuptake.
- SSRIs block this reuptake — meaning the serotonin is not taken back.
- As a result, more serotonin stays in the synapse, and it can work for a longer time.
- This extra serotonin helps reduce symptoms of depression, anxiety, and other mood problems.
In Summary: SSRIs keep more serotonin in the gap
between nerve cells and increase its effect, which helps
improve mood and reduce depression.
CNS disease product details and classification chart
Classification of CNS drugs:
Classification Chart with Brand and Generic
| Sub Class | Generic Name (ACME's Product as Example) |
|---|---|
| 1. Anxiolytic |
Clonazepam (Leptic)
Bromazepam (Tenil)
Clobazam (Cosium)
|
| 2. Anxiolytic & Antidepressant |
Flupentixol + Melitracen (Leanxit)
Amitriptyline + Chlordiazepoxide (Limbix)
|
| 3. Antidepressant |
Duloxetine HCl (Dulox)
Escitalopram Oxalate (Elodep)
|
| 4. Anti-Epileptic |
Clonazepam (Briva)
Brivaracetam (Briva)
|
| 5. Anti-Neuropathy |
Pregabalin (Neugalin)
Neugabin XR (Pregabalin)
Miraba (Mirogabalin Besyl)
|
| 6. Antiemetic & Anti-Vertigo |
Cinnarizine (Cinazin)
Cinnarizine + Dimenhydrinate (Cinazin Plus)
|
| 7. Anti-Parkinson's Disease | Levodopa + Carbidopa (Levopa) |
| 8. Memory Enhancer | Vinpocetine (Vinpoton) |
| 9. Antimigraine |
Pizotifen (Pizo-A)
Flunarizine (Fluzin)
Sumatriptan (Suma)
|
| 10. Skeletal Muscle Relaxant |
Baclofen (Skelopen)
Tolperisone HCl (A-Calm)
Prindol (Pridinol Mesilate)
|
FAQs
1. What are some widely used CNS drugs?
Some common CNS drugs include carbamazepine
(anti-epileptic), fluoxetine (anti-depressant), levodopa
(for Parkinson’s), and diazepam (for anxiety).
2. What’s the difference between a generic and a product
name?
A generic name is the actual drug name (e.g., fluoxetine),
while the product name is the brand given by a company
(e.g., Prozac).
3. How can I remember CNS drugs easily?
Group drugs by disease type and learn them with their
actions and brand names. Using charts or flashcards can help
you remember better.
4. Are CNS medicines usually long-term treatments?
Yes, many CNS conditions require long-term or even lifelong
treatment to manage symptoms and improve quality of life.
5. How does a CNS drug work in the body?
Most CNS drugs act on brain chemicals like dopamine,
serotonin, or GABA to restore balance and reduce symptoms.
6. Do CNS drugs have side effects?
Yes, like all medicines, CNS drugs may have side effects
such as dizziness, drowsiness, or mood changes. Doctors
choose drugs based on the patient’s condition.
Conclusion
Understanding CNS disease basic and product details is
essential for anyone working or planning to work as a
Medical Promotion Officer (MPO). It helps you explain
complex conditions and medicine use in simple terms. Whether
you’re talking to a doctor or learning for a pharma
interview, this foundation makes a difference. When you know
the basics well, you can grow faster in your career. This
article brings those must-know insights together for you.
So, take this chance to boost your skills and stay ahead in
your MPO journey.