Diabetes mellitus main causes: Symptoms-Types-Drugs | MPO training 23
If you’re a future Medical Promotion Officer (MPO), understanding the diabetes
mellitus main causes can help you explain treatments clearly. In this article,
you’ll learn how lifestyle, genes, and poor insulin function trigger the
disease. You will also discover the symptoms that patients often ignore.
This can give you an edge in patient discussions. Knowing the types will help
you promote the right products with confidence. Let’s make your MPO journey
more effective with these simple insights.
Table of contents: Diabetes mellitus main causes: Symptoms-Types-Drugs
Check out what you will learn from this blog-
- Diabetes mellitus main causes
- Symptoms of Diabetes Mellitus
- Types of Diabetes
- What is Insulin and How does insulin work?
- Pathological Terms
- Diabetes Diagnosis: Blood Glucose and HbA1c Thresholds
- Diabetes Management and Treatment
- DPP-4 inhibitors Mode of Action
- What are GLP-1 and GIP?
- Mode of Action of DPP-4 inhibitors + Biguanides
- Classification of Anti-Diabetic Drugs (Generic Names)
- FAQs
- Conclusion
Diabetes mellitus main causes
Diabetes mellitus mainly occurs due to insulin resistance, genetic factors,
and unhealthy lifestyle habits like poor diet and lack of exercise. Common
symptoms include frequent urination, fatigue, and unexplained weight loss.
There are two main types: Type 1 and Type 2. Each type affects insulin
differently. Understanding these helps Medical Promotion Officers (MPOs)
provide better drug information to doctors and patients.
We will now learn about the above topics step by step.
What is Diabetes?
Diabetes mellitus (DM), commonly known as diabetes. Diabetes is a lifelong
(chronic) disease in which there are high levels of sugar in the blood.
How does diabetes mellitus affect the body?
Diabetes mellitus is a chronic condition where your body can’t use insulin
properly, or doesn’t make enough of it. This causes high blood sugar
levels, which can slowly damage your heart, kidneys, eyes, and nerves over
time.
Which organs are most affected by diabetes mellitus?
Diabetes mainly affects the heart, kidneys, eyes, brain, and nerves. Over
time, high blood sugar slowly damages blood vessels and leads to poor
function of these organs.
Main Cause of Diabetes Mellitus
The main cause of diabetes mellitus is related to how your body handles
insulin, the hormone responsible for controlling blood sugar levels.
It usually happens due to one of the following two reasons:
- Insulin Deficiency – When your pancreas fails to produce enough insulin. This condition is commonly seen in Type 1 diabetes.
- Insulin Resistance – When your body’s cells do not respond properly to insulin. This is more common in Type 2 diabetes.
As a result of either problem, glucose builds up in the blood instead of
entering the cells, leading to high blood sugar levels (hyperglycemia).
This is the core reason why managing insulin function is so important in
the treatment and prevention of diabetes mellitus.
Diabetes Mellitus: Global Statistics and Growing Concern
Diabetes mellitus is not just a single disease — it’s a growing global
health crisis.
According to the International Diabetes Federation (IDF) Diabetes Atlas
2024:
- Over 537 million adults (aged 20–79) are living with diabetes worldwide.
- By 2045, this number is expected to reach 783 million, if no major actions are taken.
- About 1 in 10 adults globally now has diabetes, and nearly half of them don’t even know they have it.
- Type 2 diabetes accounts for around 90% of all diabetes cases, and it’s mostly linked to poor lifestyle, obesity, and aging.
- In low- and middle-income countries, diabetes is rising at a much faster rate compared to high-income countries.
Sources: International Diabetes Federation (IDF) Atlas – 10th
Edition, 2024, WHO Global Report on Diabetes and World Bank Data (for
income-based analysis).
This rapid rise in diabetes is a big concern not only for patients but
also for healthcare systems and professionals. For a Medical Promotion
Officer (MPO), understanding these facts is essential when promoting
anti-diabetic drugs or educating doctors.
Symptoms of Diabetes Mellitus
Diabetes mellitus causes several symptoms because your body cannot
properly control blood sugar levels.
You may notice:
- Polyuria (Frequent urination): You feel the need to urinate more often than usual.
- Polydipsia (Excessive thirst): You become very thirsty and want to drink a lot of water.
- Polyphagia (Increased hunger): You feel hungry more often and eat more than usual.
- Hyperglycemia (High blood sugar): Your blood contains too much sugar.
- Glycosuria (Sugar in urine): Extra sugar leaves your body through urine.
- Asthenia (Weakness): You feel tired and weak.
- Weight loss: You may lose weight even if you eat well.
- Fatigue: You feel very tired during the day.
- Blurred vision: Your eyesight may become unclear or fuzzy.
- Slow healing wounds: Cuts or sores take a long time to heal.
- Frequent infections: You get infections often, especially skin or urinary tract infections.
- Tingling or numbness: You may feel pins and needles or numbness in your hands or feet.
- Dry and itchy skin: Your skin may become dry and itchy.
- Dark patches on the skin: You might notice dark, thickened skin patches, usually on the neck or underarms.
- Mood changes: You might feel irritated or moody at times.
- Nausea or vomiting: Sometimes, especially in Type 1 diabetes, you may feel sick or vomit.
If you notice any of these symptoms, it’s important to see a doctor for
testing. As a Medical Promotion Officer (MPO), knowing these signs helps
you support patients better and promote the right medicines effectively.
Types of Diabetes
There are three major types of diabetes:
- Type 1 diabetes (IDDM)
- Type 2 diabetes (NIDDM)
- Gestational diabetes
1. Type 1 Diabetes- Insulin-Dependent Diabetes Mellitus
(IDDM): In this disease, the body makes little or no insulin. Daily injections of
insulin are needed. Can occurs at any age, but it is most often diagnosed
at an early age (20-35). Also called Juvenile Diabetes.
2. Type 2 Diabetes- Non-Insulin Dependent Diabetes
Mellitus (NIDDM):
Type 2 diabetes is a long-term metabolic disorder that is characterized by
high blood sugar, insulin resistance, and relative lack of insulin. Type 2
diabetes usually begins at a late part of life & patients become
obese.
3. Type 3 Diabetes- Gestational Diabetes: Blood sugar
levels are high during pregnancy in women. High risk of type 2 diabetes
and cardiovascular disease.
Difference between Type 1 & Type 2 Diabetes Mellitus
| FEATURE | Type 1 DM | Type 2 DM |
|---|---|---|
| Pathogenesis | Body is no longer able to produce Insulin - Insulin deficiency | Body produces insulin but does not enough use of it- Insulin resistance |
| Prevalence | 10-20% population | 80-90% population |
| Age at onset | Usually starts at early age (20-35 years) | Most commonly after 40 years |
| Type of onset | Abrupt and severe | Gradual & insidious |
| Risk Factor | Family History | Over weight, less physical activity, Family History |
| Symptoms | Blurry vision, Frequent Urination, mode change, irritability, Increased thirst | Increase appetite & thirst, Frequent Urination, Tiredness, weight gain, delay in wound healing |
| Treatment | Insulin, healthy lifestyle | OAD, Insulin, healthy lifestyle |
What is Insulin and How does insulin work?
What is the role of insulin in diabetes mellitus?
Insulin helps move sugar from your blood into cells for energy. In
diabetes mellitus, either your body doesn’t make insulin (Type 1) or
doesn’t use it properly (Type 2), causing high blood sugar levels.
Insulin: Insulin is a peptide hormone produced by beta cells of
the pancreatic islets. It is considered to be the main anabolic hormone
of the body. It regulates the metabolism of carbohydrates, fats and
protein by promoting the absorption of glucose from the blood into
liver, fat and skeletal muscle cells.
How does insulin work?
After you eat, your blood sugar (glucose) rises. This rise in glucose
triggers your pancreas to release insulin into the bloodstream. Insulin
travels through the blood to your body's cells. It tells the cells to
open up and let the glucose in. Once inside, the cells convert glucose
into energy or store it to use later.
Pathological Terms
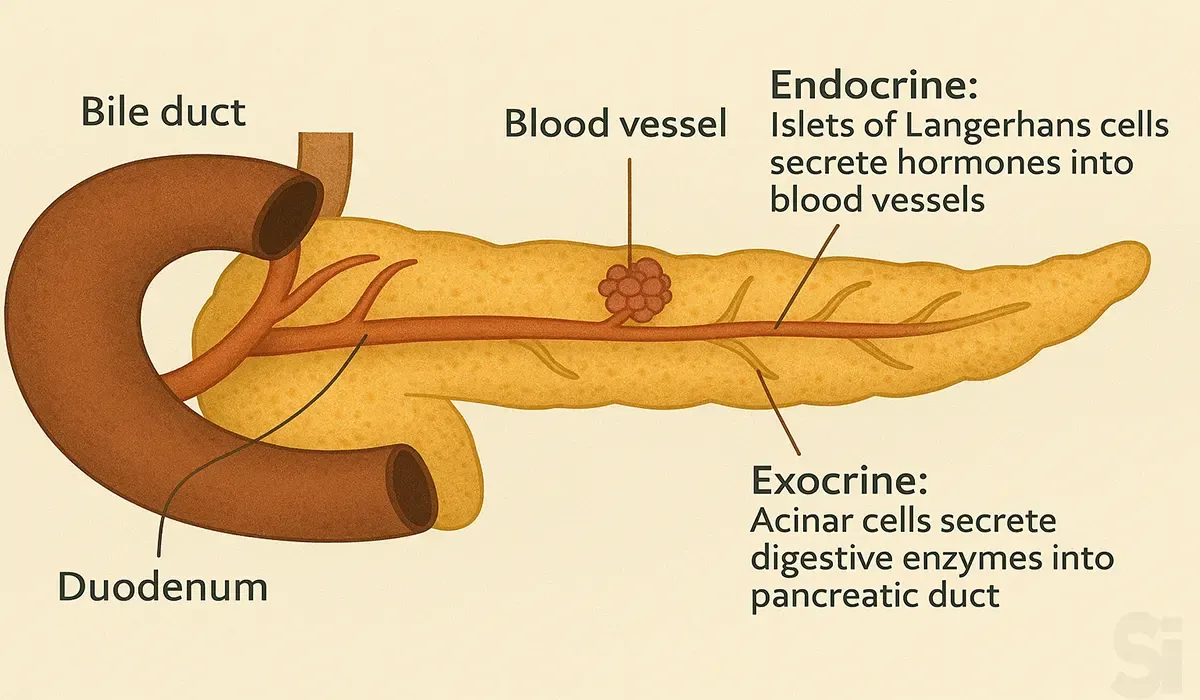
Pancreas: The pancreas is an organ located in the abdomen. It
plays an essential role in converting the food we eat into fuel for the
body's cells.
The pancreas has two main functions: an exocrine function that helps in
digestion and an endocrine function that regulates blood sugar.
Insulin deficiency: Lack of insulin production. It occurs when
insulin-producing cells are damaged or destroyed and stop producing
insulin.
Insulin Resistance: The inability of cells to respond to the
action of insulin in transporting glucose (sugar) from the bloodstream
into muscle and other tissues.
Glucagon: Glucagon Is a hormone secreted from alpha cells of
pancreases that increases in blood sugar level.
Glycogen: Glycogen Is a stored form of glucose. It is stored
mainly in the liver and the skeletal muscles.
Gluconeogenesis (GNG): Gluconeogenesis is a metabolic
pathway that results in the generation of glucose from certain
non-carbohydrate carbon substrates.
DPP-4: Dipeptidyl peptidase-4, An enzyme responsible for the
degradation of incretin hormones.
Incretin Hormone: It is a group of metabolic hormones. It is
released after eating and helps the secretion of insulin. Glucagon-like
peptide-1 (GLP-1))and Glucose-dependent insulinotropic polypeptide (GIP)
are Incretin Hormones.
HbA1c: Glycated Hemoglobin. It is the amount of blood sugar
(glucose) attached to hemoglobin.
Hypoglycemia: Low blood sugar (glucose), when blood sugar
drops below normal levels.
- Normal Blood Sugar level: 4.0 to 5.4 mmol/L (72 to 99 mg/dL).
- Hypoglycemia- Blood sugar level below 3.9 mmol/L (70 mg/dL).
Hyperglycemia: High blood sugar or excessive amount of glucose
circulates in the blood plasma.
- Hyperglycemia- Blood sugar level upper 7 mmol/L (126 mg/dL) during fasting.
Diabetes Diagnosis: Blood Glucose and HbA1c Thresholds
| Condition | Unit (mmol/L) | Unit (mg/dL) |
|---|---|---|
| Normal | less than 5.6 mmol/L | less than 100 mg/dL |
| Prediabetes | 5.6 to 6.9 mmol/L | 100 to 125 mg/dL |
| Diabetes | higher than 7 mmol/L | higher than 126 mg/dL |
| Condition | Unit (mmol/L) | Unit (mg/dL) |
|---|---|---|
| Normal | less than 7.8 mmol/L | less than 140 mg/dL |
| Prediabetes |
between 7.8 mmol/L to 11.0 mmol/L |
between 140 and 199 mg/dL |
| Diabetes | more than 11.1 mmol/L | more than 200 mg/dL |
Hemoglobin A1c test (HbA1c):
- Normal: Less than 5.7%
- Pre-diabetes: 5.7% - 6.4%
- Diabetes: 6.5% or higher
Diabetes Management and Treatment
How does diabetes mellitus affect daily life and work?
People with diabetes need to monitor blood sugar, eat regularly, and
take medicines. With proper care, most can live a normal life, but
ignoring the condition may reduce energy and focus at work.
A) Management:
Unfortunately, there is currently no permanent cure for diabetes.
However, it can be effectively managed through a combination of
healthy lifestyle choices, regular monitoring, and medical treatment.
The goal is to maintain blood glucose levels within the target range
and prevent or delay complications.
Core Principles of Diabetes Management – The 5 D’s:
1. Discipline:
- Regular monitoring of blood sugar.
- Adherence to lifestyle changes.
- Consistency in daily routine.
- Stress reduction and mental well-being.
2. Diet:
- Balanced meals with controlled carbohydrates.
- High fiber, low sugar, and low saturated fats.
- Regular meal times and portion control.
- Avoidance of processed and sugary foods.
3. Drugs:
- Oral hypoglycemic agents (OHAs) for Type 2 diabetes.
- Insulin therapy (especially for Type 1 diabetes or advanced cases).
- Medication compliance is critical to long-term success.
4. Daily Exercise:
- At least 30 minutes of moderate physical activity (e.g., walking, cycling) most days of the week.
5. Doctor Visits:
- Regular checkups
- Monitoring of HbA1c, kidney function, eyes, and feet to catch complications early.
B) Treatment of Diabetes
Treatment of diabetes depends on the type of diabetes, the
severity, and the individual’s health condition. The primary goal
is to control blood sugar levels and prevent complications.
1. Type 1 Diabetes Treatment:
- Requires daily insulin therapy (injections or insulin pump).
- Blood glucose monitoring multiple times a day.
- May include carbohydrate counting and meal planning.
2. Type 2 Diabetes Treatment:
- Begins with lifestyle changes: healthy eating, physical activity, and weight management.
- If lifestyle alone is not sufficient, oral medications (oral hypoglycemic agents) are prescribed.
- In advanced stages or if oral drugs fail, insulin may be added.
- Other medications may also be used to protect the heart, kidneys, or lower cholesterol and blood pressure.
3. Gestational Diabetes Treatment:
- Focuses on healthy diet and physical activity during pregnancy.
- If blood sugar remains high, insulin or oral medications may be recommended.
- Careful monitoring of mother and baby is essential.
Common Medications Used in Treatment:
- Metformin – First-line drug for type 2 diabetes.
- Sulfonylureas (e.g., glipizide, glyburide) – Stimulate insulin release.
- DPP-4 inhibitors, GLP-1 receptor agonists, SGLT2 inhibitors – Newer classes for better control and heart/kidney protection.
- Insulin – Various types: rapid, short, intermediate, and long-acting.
Important Notes: Always follow your doctor's advice for
medication and dosing. Never stop or change medication without
medical consultation. Self-monitoring of blood glucose (SMBG)
is vital to ensure treatment effectiveness. Treatment must be
individualized—there is no one-size-fits-all approach.
What lifestyle changes help manage diabetes mellitus
effectively?
Eating a balanced diet, regular exercise, reducing stress,
maintaining weight, quitting smoking, and routine blood
sugar checks are key lifestyle changes that improve diabetes
control.
DPP-4 inhibitors Mode of Action
Step-by-Step Explanation of the Diagram: This diagram
illustrates how DPP-4 inhibitors (a type of diabetes medication) work
in the body.
Step 1: Food intake
- When we eat food, our body produces incretin hormones.
Step 2: Incretin hormones
- These hormones perform two main functions:
- Stimulate insulin release → Increases insulin secretion.
- Inhibit glucagon release → Decreases glucagon (a hormone that raises blood sugar levels).
Step 3: Result – Lowering of blood glucose
- The combined effect of increased insulin and decreased glucagon leads to reduced blood glucose levels.
Step 4: The Problem – DPP-4 enzyme
- The body naturally produces an enzyme called DPP-4, which inactivates incretin hormones.
- This reduces the beneficial effects of increments.
Step 5: The Solution – DPP-4 Inhibitors
- DPP-4 inhibitors are medications that block the DPP-4 enzyme.
- As a result, incretin hormones remain active for a longer time.
- This leads to increased insulin release, decreased glucagon levels, and ultimately lower blood sugar.
In Summary: DPP-4 inhibitors are drugs that keep incretin
hormones active longer, thereby boosting insulin, reducing glucagon,
and lowering blood glucose levels.
What are GLP-1 and GIP?
GLP-1 (Glucagon-Like Peptide-1): GLP-1 is a natural
hormone released from the intestines after we eat.
What it does:
- Stimulates the body to release insulin (which lowers blood sugar).
- Reduces glucagon, a hormone that increases blood sugar.
- Slows down stomach emptying, which helps to reduce appetite.
GIP (Glucose-dependent Insulinotropic Polypeptide): GIP
is another incretin hormone also released after eating.
What it does:
- Increases insulin release only when blood sugar is high (this is why it's called glucose-dependent).
- Helps reduce glucose production in the liver.
In Summary: GLP-1 and GIP are both hormones that help
increase insulin release after eating and lower blood sugar. Keeping
these hormones active helps the body control blood sugar better.
That’s why DPP-4 inhibitor medicines are useful — they prevent these
hormones from being broken down, allowing them to work longer.
| Feature/Function | GLP-1 (Glucagon-Like Peptide-1) | GIP (Glucose-dependent Insulinotropic Polypeptide) |
|---|---|---|
| Where it is released from | Small intestine (after eating) | Small intestine (after eating) |
| Stimulates insulin release? | ✅ Yes | ✅ Yes (only when blood glucose is high) |
| Suppresses glucagon? | ✅ Yes (reduces blood sugar further) | ❌ No major effect |
| Slows down stomach emptying? | ✅ Yes (helps control appetite) | ❌ No |
| Effect on liver glucose production | Indirectly reduced (via insulin action) | ✅ Helps reduce liver glucose output |
| Short lifespan in body? | Yes – quickly broken down by DPP-4 enzyme | Yes – also broken down by DPP-4 |
| Supported by DPP-4 Inhibitors? | ✅ Yes – works longer when DPP-4 is blocked | ✅ Yes – works longer when DPP-4 is blocked |
Summary (Easy to Remember):
- GLP-1 helps with insulin release, lowers glucagon, and reduces appetite.
- GIP helps with insulin release and reducing liver glucose, but only when sugar is high.
- Both are broken down by the DPP-4 enzyme, so using DPP-4 inhibitors keeps them active longer and helps control diabetes.
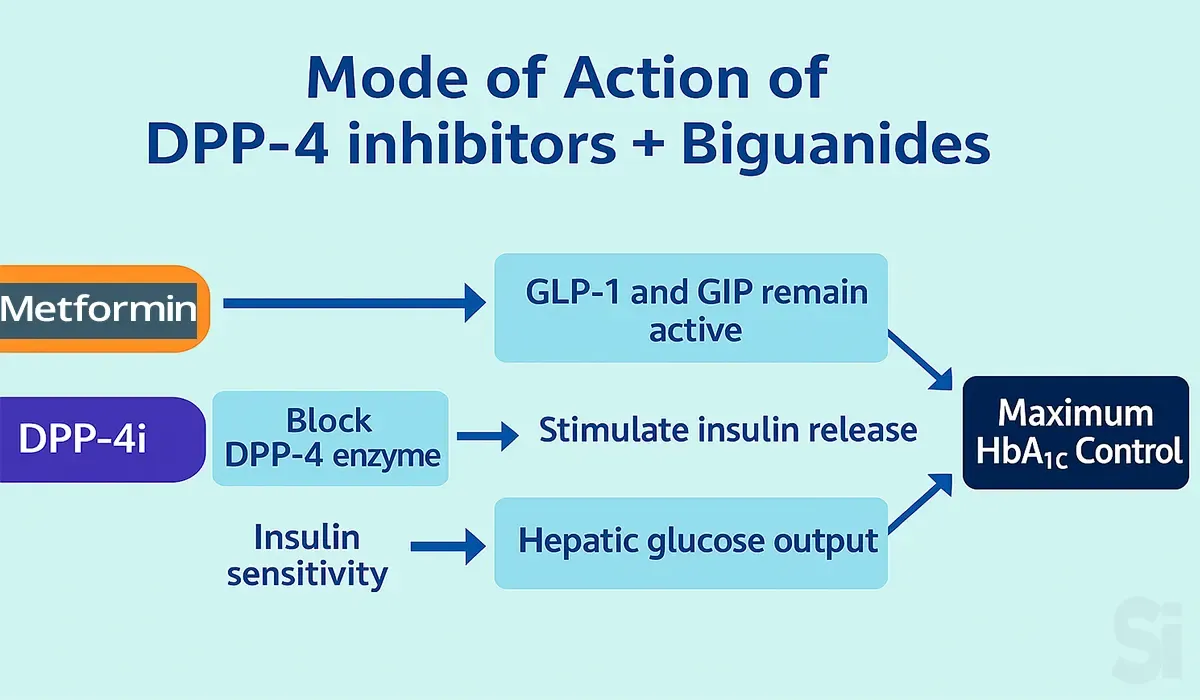
Mode of Action of DPP-4 inhibitors + Biguanides
DPP-4 Inhibitors work by inhibiting the DPP-4 enzyme which in
turn increases the incretin hormone levels (GLP-1 & GIP) by
preventing the breakdown of GLP-1 & GIP & Biguanides
increase insulin sensitivity and decreases hepatic glucose
overproduction.
What the Image Explains – Step-by-Step Explanation:
Step 1: Metformin (a type of Biguanide medicine)
- Metformin helps keep GLP-1 and GIP (incretin hormones) active in the body.
Step 2: DPP-4 Inhibitors (DPP-4i)
- These medicines block the DPP-4 enzyme, so incretin hormones stay active longer.
- As a result, the body releases more insulin.
Step 3: Insulin Sensitivity
- Metformin also improves insulin sensitivity, which helps the liver produce less glucose (this is called reducing hepatic glucose output).
Step 4: Combined Effect
- Together, Metformin and DPP-4 inhibitors help control blood sugar better by reducing glucose levels and increasing insulin — which leads to better control of HbA1c (a long-term marker of blood sugar control).
Summary: This image clearly shows how Metformin + DPP-4
inhibitors work together to control blood sugar levels and help
maintain a healthy HbA1c.
Classification of Anti-Diabetic Drugs (Generic Names)
| Sub-Class / Group | Generic Names |
|---|---|
| - |
Short-acting: Regular Insulin
Intermediate-acting: NPH Insulin
Long-acting: Insulin Glargine, Insulin Detemir,
Insulin Degludec
Rapid-acting: Insulin Lispro, Insulin Aspart,
Insulin Glulisine
|
| Sub-Class / Group | Generic Names |
|---|---|
| 1. Biguanides | Metformin |
| 2. Sulfonylureas | Glimepiride, Gliclazide, Glibenclamide (Glyburide), Glipizide |
| 3. Meglitinides | Repaglinide, Nateglinide |
| 4. Thiazolidinediones (TZDs) | Pioglitazone, Rosiglitazone |
| 5. DPP-4 Inhibitors | Sitagliptin, Vildagliptin, Linagliptin, Alogliptin, Saxagliptin, Teneligliptin |
| 6. SGLT-2 Inhibitors | Empagliflozin, Dapagliflozin, Canagliflozin, Ertugliflozin |
| 7. Alpha-glucosidase inhibitors | Acarbose, Miglitol |
| 8. GLP-1 Receptor Agonists | Semaglutide, Liraglutide, Dulaglutide, Exenatide |
| 9. Amylin analogs | Pramlintide |
| 10. Dual GIP/GLP-1 Agonists | Tirzepatide |
In this chart, it is shown that Metformin (one of the most
common diabetes medications) works better when used in
combination with other drugs.
These mixed-use medications are called "Combination Therapy."
1. DPP-4 Inhibitor + Metformin: DPP-4 inhibitors are
drugs that keep the body's incretin hormones active for
longer, which increases insulin secretion and reduces blood
glucose levels.
The following combinations are commonly used with
Metformin:
- Sitagliptin + Metformin
- Vildagliptin + Metformin
- Linagliptin + Metformin
These combinations are often made by pharmaceutical companies
as single tablets containing both drugs.
2. SGLT-2 Inhibitor + Metformin: SGLT-2 inhibitors are
drugs that remove excess glucose from the body through urine,
thus lowering blood sugar levels.
The combination mentioned:
- Empagliflozin + Metformin
This combination is also available as a single tablet.
Summary in Table Format (Only Generic Names):
| Combination Type | Generic Combination | Function |
|---|---|---|
| DPP-4 Inhibitor + Biguanide |
Sitagliptin + Metformin Vildagliptin + Metformin Linagliptin + Metformin |
Increases insulin secretion, lowers blood glucose |
| SGLT-2 Inhibitor + Biguanide | Empagliflozin + Metformin | Removes glucose through urine, lowers blood glucose |
FAQs
1. What causes diabetes mellitus in adults and
children?
In adults, poor lifestyle choices, obesity, and genetic
factors often lead to Type 2 diabetes. In children, Type 1
diabetes is usually caused by an autoimmune reaction where
the body attacks its own insulin-producing cells.
2. How is diabetes mellitus different from diabetes
insipidus?
Diabetes mellitus is related to blood sugar problems, while
diabetes insipidus is a rare condition involving water
balance and kidney function. They share the name "diabetes"
but are completely different diseases.
3. What are the early warning signs of diabetes
mellitus?
Early symptoms include frequent urination, excessive thirst,
tiredness, blurry vision, slow wound healing, and unexpected
weight loss. These signs should not be ignored and need
medical attention.
4. How is diabetes mellitus diagnosed by doctors?
Doctors usually perform blood tests such as fasting blood
glucose, HbA1c, and oral glucose tolerance tests to diagnose
diabetes mellitus. These tests help check your blood sugar
levels over time.
5. What are the long-term complications of uncontrolled
diabetes mellitus?
If not managed well, diabetes can lead to serious
complications like heart disease, stroke, kidney failure,
blindness, nerve damage, and foot ulcers that may require
amputation.
6. Can diabetes mellitus be reversed or cured?
Type 1 diabetes cannot be cured. Type 2 diabetes may go into
remission with lifestyle changes, weight loss, and proper
treatment, but it’s not considered a permanent cure.
Conclusion: Diabetes mellitus main causes
To sum up, understanding the diabetes mellitus main causes:
symptoms and types gives you a strong base as a future MPO.
This knowledge helps you speak confidently with healthcare
professionals. Whether it’s Type 1 or Type 2, knowing what
triggers the condition can guide your approach. As a Medical
Promotion Officer, such insights can shape your daily
activities. Keep learning to make your role more meaningful.
This knowledge isn’t just medical—it’s your tool for
building trust.